Learn why stem cell replacement therapy for dry macular degeneration is showing promise.
Dry Age-Related Macular Degeneration
According to a study by the National Medical Research Council in Singapore, an estimated 196 million people suffer from age-related macular degeneration (AMD), and this number is projected to increase to 288 million by 2040. AMD is the leading cause of blindness among people over the age of 55 in the U.S. and Europe.
Unfortunately, there are presently no treatments to completely cure this disease. Photoreceptors, the light-sensing nerve cells present in the retina of the eye, die during the progression of AMD, which leads to vision loss. These photoreceptors rely on nourishment and maintenance from the retinal pigment epithelium (RPE), a single-cell layer that lies behind the retina.
Current research indicates that RPE dysfunction is a major driver of AMD development. Once the photoreceptors are lost, it is difficult for patients to perform their normal daily activities.
Dry AMD is the most common subtype of this disease, distinguished from wet AMD by the lack of blood vessel leakage in the retina. Due to the absence of such complications, dry AMD provides better opportunities for treatment.
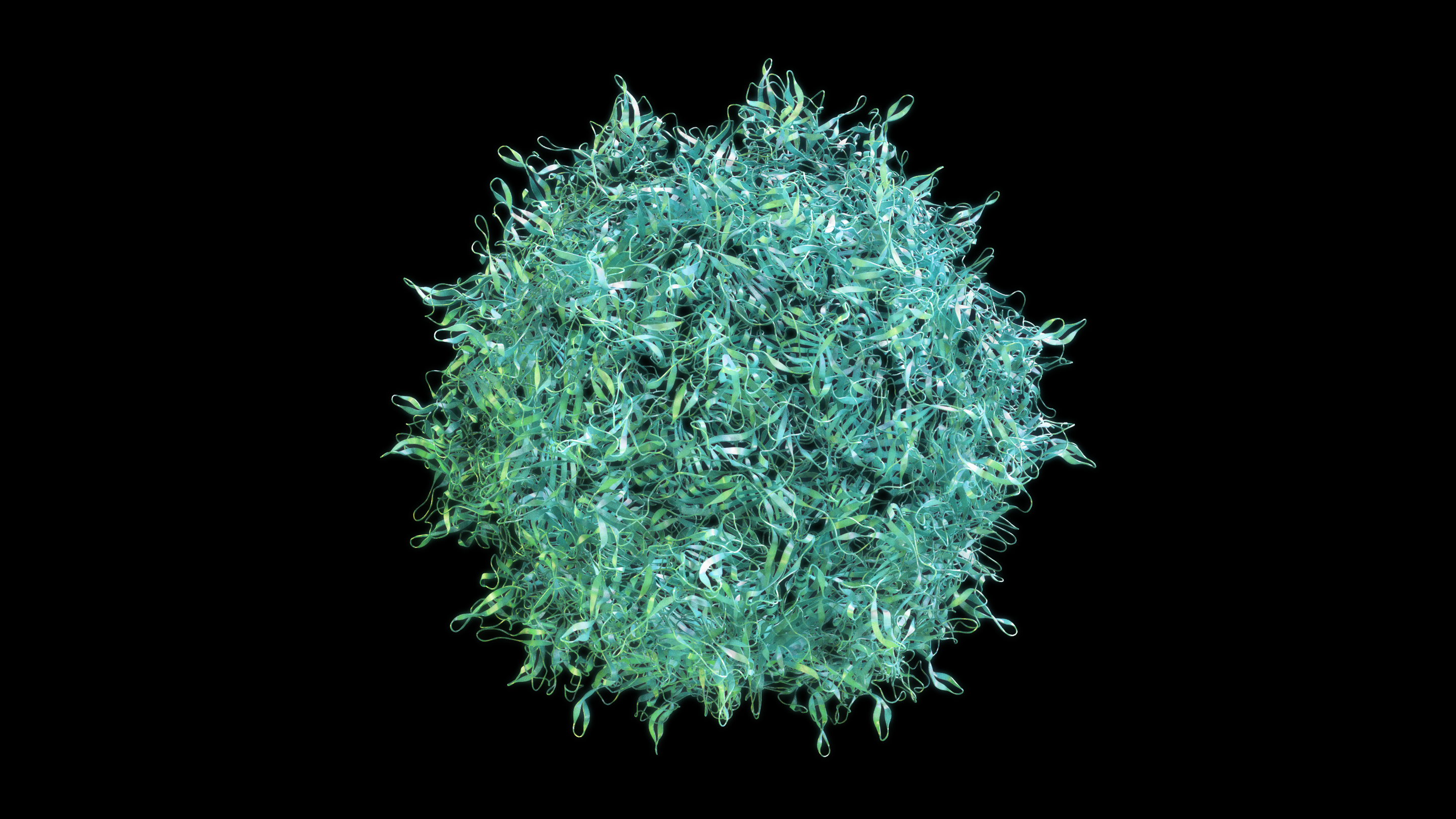
Stem Cell-Based Treatment Strategies for Dry AMD
Stem cell therapy provides great hope for curing degenerative eye diseases like dry AMD. The benefit of cell replacement therapies for AMD patients can be obtained through two possible avenues:
- healthy transplanted cells can release factors that rejuvenate dysfunctional RPE and photoreceptors, or
- cell replacement can directly replace dysfunctional cells.
Based on preclinical studies, the positive effects of stem cell transplants are likely a combination of both of these factors. During the early stages of dry AMD, since photoreceptors are well preserved, and disease progression is mostly limited to the RPE, treatment strategies can focus on reversing RPE dysfunction, which is comparatively easy to accomplish.
For direct cell replacement therapies in the eye, RPE transplantation is a relatively easy and straightforward approach. The RPE can be derived from stem cells and can be grown with structural and functional similarities to the RPE in the eye. This RPE is then transplanted, integrates into the host retina, and supports photoreceptor functionality, demonstrating faithful replacement of the diseased RPE. Preclinical studies attribute the improved visual function achieved in their experiments to the survival and functionality of transplanted RPE.
Current Status of Stem Cell Therapies for Dry AMD
Current treatment for dry AMD using stem cells is mostly based on RPE replacement strategies. Since the RPE supports photoreceptors, RPE replacement can alleviate visual functional deficits by reinstating photoreceptor functionality. Attempts have been made to use a patient’s own cells to generate iPSCs and minimize immunological issues associated with transplantation. Studies conducted in AMD patients demonstrated that transplanted cells survive in the host eye and contribute to visual functional improvement. Most importantly, no adverse events such as transplant rejection or tumor formation were observed in any of these patients.
Prospects of Stem Cell Therapies for Dry AMD Patients
Although RPE replacement therapies showed promising results in AMD patients, no strategies have been developed to perform photoreceptor replacement therapy, a requirement for late-stage AMD patients whose vision is compromised due to severe photoreceptor loss.
Various groups have conducted photoreceptor transplantation studies in animal models, but there is a lack of supportive data to translate this approach to human clinical trials. Unlike the RPE, the survival and functionality of photoreceptors is a more difficult approach to accomplish success.
Recent studies on stem cells that are committed to forming photoreceptor cells and 3D stem cell-derived retinal tissue suitable for grafts show promise in preclinical studies. These studies demonstrated the safety and efficacy of these approaches and their potential to reverse blindness.
Important Clinical Trial Information
People who might be interested in enrolling in a cell transplantation clinical trial should ask their ophthalmologist about their eligibility and the current availability of trials. Under no circumstances should patients have cell transplantation or injection outside the protections of a clinical trial registered on clinicaltrials.gov or Antidote. Recently, stem cell injections into the eye, offered by a clinic but not part of a registered clinical trial, resulted in catastrophic vision loss due to the lack of proper regulatory approval. For more information on this issue, visit here.
Conclusion
Stem cell replacement therapy for dry AMD patients, which currently consist of RPE transplantation alone, is showing great promise. Various research groups are actively involved in developing this technique into a routine clinical procedure. There is still much work to be done before a stem cell therapy for advanced-stage dry AMD that replaces both the RPE and photoreceptors can be fully developed.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Clinical Trials
- Disease Biology
- Treatments