Wet Macular Degeneration
Over time, dry macular degeneration can progress to a more serious form called wet macular degeneration.

What is it?
What Is Wet Age-Related Macular Degeneration?
Wet macular degeneration accounts for approximately 10 percent of the cases of age-related macular degeneration. However, it results in 90 percent of the cases of legal blindness. All wet macular degeneration is considered advanced

How it happens:
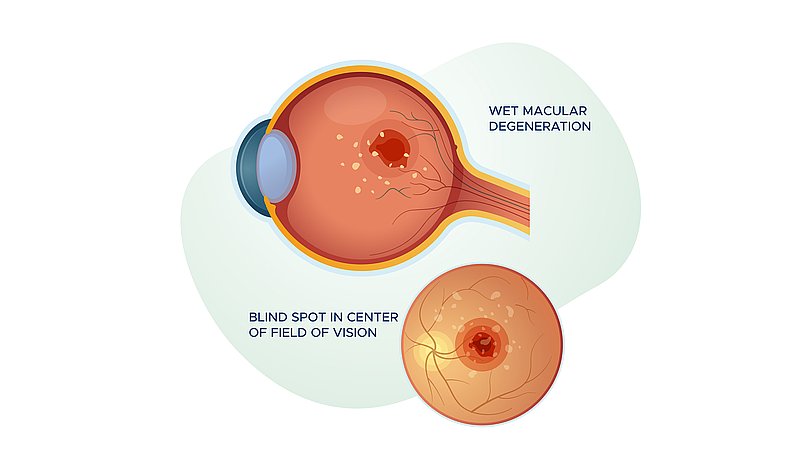
- Wet AMD occurs when abnormal blood vessels grow behind the macula as retinal pigmented epithelium (RPE) and photoreceptor cells die.
- Bruch’s membrane begins to break down, usually near drusen deposits, and new blood vessels grow. This growth is called neovascularization.
- These vessels are very fragile and leak fluid and blood, resulting in scarring of the macula and the potential for rapid, severe damage. This causes the retina to become “wet.”
- Straight-ahead vision can become distorted or lost entirely quickly, sometimes within days or weeks.
Symptoms
Wet AMD Symptoms
Initially, the leaking fluid into the retina causes reversible vision loss, but the vision loss can become permanent within weeks to months if untreated. This is why it’s very important to detect wet macular degeneration as soon as possible.
Wet macular degeneration symptoms include:
- Sudden leaking into the retina. (This process is painless.)
- Distortion or a blind spot in the central vision– the blind spot can appear gray, red, or black.
People with wet AMD may be diagnosed with early-stage dry AMD years before wet AMD occurs.
Testing
Diagnostic Tests for Wet Macular Degeneration
First, your ophthalmologist will perform a dilated eye exam and optical coherence tomography (OCT) imaging to determine whether you have wet macular degeneration. If so, you will likely benefit from a series of injections, initially spaced every four to six weeks (perhaps less frequently later on depending on how your eye responds).
Fluorescein Angiography
If your doctor suspects you may have wet AMD, he or she may conduct this test to detect leaking blood vessels. The doctor injects fluorescent dye into your arm and traces it through the blood vessels in the retina, where the appearance of fluorescent patches can reveal leakage.
Treatments
Treating Wet AMD
While there is no cure for wet AMD, there are treatment options that may slow the rate of vision decline or further loss. However, the disease and loss of vision may also progress despite treatment. Options should be discussed with your doctor.
Wet macular degeneration is most commonly treated with injections of angiogenesis inhibitors into the eye, photodynamic therapy, or laser surgery, which all slow the growth of new, fragile, and often leaky blood vessels.
Anti-VEGF and Other Injected Treatments
Years of intensive research revealed that the retinas of some people with macular degeneration secrete too much of a protein called vascular endothelial growth factor (VEGF), causing the growth and leakage of the blood vessels. This process can be slowed or stopped by injecting drugs into the eye that bind and inhibit VEGF. Anti-VEGF shots block vascular endothelial growth factor, a key molecule in the production of new blood vessels in a process called angiogenesis, and are injected into the back of the eye, which has been numbed beforehand.
Photodynamic Therapy
- Photodynamic therapy (PDT) is most effective in a subtype of wet AMD called predominantly classic subfoveal AMD, in which blood vessel growth and leakage in the fovea—the small region in the center of the macula—are well defined. It should be noted that PDT is rarely used now that there are drugs (Eylea, Lucentis, and Avastin) that specifically block the vessel-promoting VEGF protein.
- During the PDT procedure, a drug called Visudyne is injected into the arm. The drug courses through the body and is absorbed by the fragile, leaking blood vessels in the eye. Because Visudyne is activated by light, the doctor directs a low-intensity laser at the retina for a little over a minute. The light activates the Visudyne, allowing it to destroy the abnormal vessels without harming healthy blood vessels. PDT may help to stabilize vision, but it will not restore lost vision.
Laser Surgery
Laser photocoagulation surgery was the first treatment used for wet AMD, but it is appropriate only for a small subset of people. This treatment is not as commonly used as angiogenesis inhibitors. A laser is used to destroy the leaky blood vessels that threaten to damage the eye. This surgery can prevent further vision loss but results in a permanent blind spot.

Monitoring
Monitoring Your Vision
Considering wet AMD evolves from dry macular degeneration, a best practice is to regularly see your eye doctor as well as monitor your vision at home and share any changes with your doctor.
Early macular degeneration symptoms are subtle.
Even if you have not been diagnosed with macular degeneration, you should have a dilated eye exam every year or two once you reach the age of 55 to detect early signs of the disease.
Monitor your vision at home.
If you have been diagnosed with dry AMD, you can detect changes in your vision, like a blind spot or distortion, using an Amsler grid eye test—a simple tool you can use from the comfort of home.
Note that it sometimes can be difficult to distinguish a central blind spot from “floaters.”
Definitions
Wet AMD Glossary
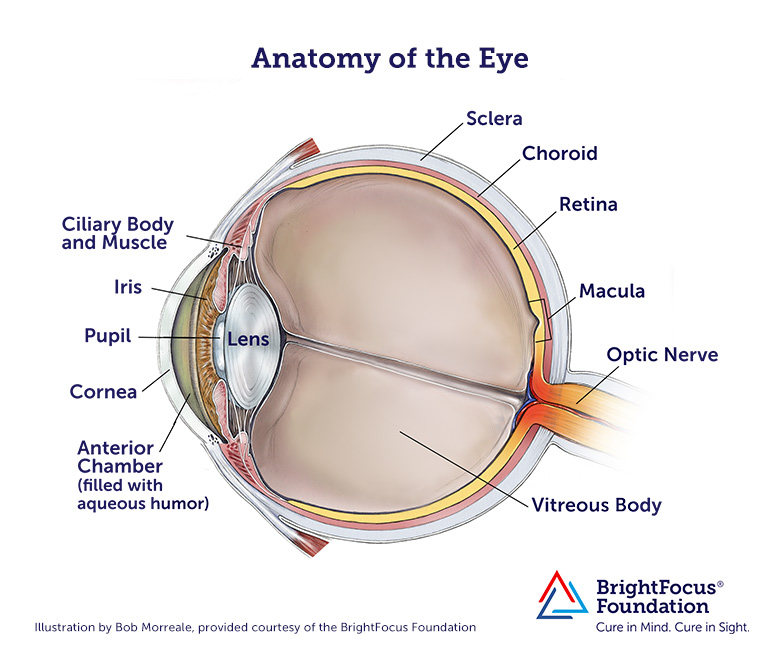
Bruch’s membrane
Located in the retina between the choroid and retinal pigmented epithelium (RPE) layer; provides support to the retina and functions as the ‘basement’ membrane of the RPE layer.
Choroid
Layer of the eye behind the retina; contains blood vessels that nourish the retina.
Cones
The photoreceptor nerve cells present in the macula and concentrated in the fovea (the very center of the macula); enable people to see fine detail and color.
Drusen
Deposits of yellowish extracellular waste products that accumulate within and beneath the retinal pigmented epithelium (RPE) layer.
Fovea
The pit or depression at the center of the macula that provides greatest visual acuity.
Macula
The portion of the eye at the center of the retina that processes sharp, clear, straight-ahead vision.