Age-related macular degeneration (AMD) is a common condition among those over the age of 50. Patients with early macular degeneration typically have no symptoms. As it progresses, it begins to affect the ability to read, write, and drive. Currently, it is the leading cause of central vision loss in the United States. There are two types of macular degeneration; the more common dry form and a wet form.
The hallmark of dry AMD is the presence of drusen. Drusen are yellow deposits underneath the retina that are visible to your physician during a dilated eye examination. Many patients with drusen have no symptoms and no vision loss. With dry macular degeneration, the rate of vision loss is very gradual. For some, dry macular degeneration can progress to affect the central vision and cause blurring of vision over time. Currently, there are no treatments for dry macular degeneration but there are many things a patient can do to decrease their chance of progression.
Risk Factors
Genetics has a crucial role in the development of macular degeneration. Many genetic markers exist that can predict the risk of progression and can assess severity. Genetic testing is available and can identify patients who are at higher risk of developing advanced AMD.
Environmental factors have also been identified. While age, race, and genetics cannot currently be modified, there are many things that patients can avoid, such as eating an unhealthy diet and smoking. Eating fresh green vegetables and avoiding a diet rich in processed foods and fats are important in the prevention of advanced forms of macular degeneration. A diet of dark green leafy vegetables and omega-3 fatty acids helps to decrease the inflammation that is associated with AMD. On the contrary, patients who are obese, have uncontrolled high blood pressure, or are current smokers have over a two to three times risk of advanced AMD.
After Diagnosis
Fortunately, only 10-15% of patients with dry macular degeneration progress to wet macular degeneration. Wet AMD is characterized by more abrupt central vision loss caused by abnormal blood vessels that bleed or leak fluid. Even with wet AMD, patients rarely go totally blind because the peripheral vision remains unaffected. Most symptoms include difficulty reading, distortion, and blurry central vision. The Age-Related Eye Disease Study (AREDS2) identified supplements that can be taken in patients with dry AMD who are at higher risk of developing wet AMD. The AREDS2 formula includes vitamins C and E with anti-oxidants Lutein and Zeaxanthin along with zinc that decrease the progression to more advanced forms of AMD.
Home Monitoring
In addition to regular eye examinations, home monitoring has been proven to improve the detection of wet AMD. Fortunately, there are numerous medications available for wet AMD, but they work best when given as early as possible, and early detection remains key. Traditionally, home monitoring is done with an Amsler grid.
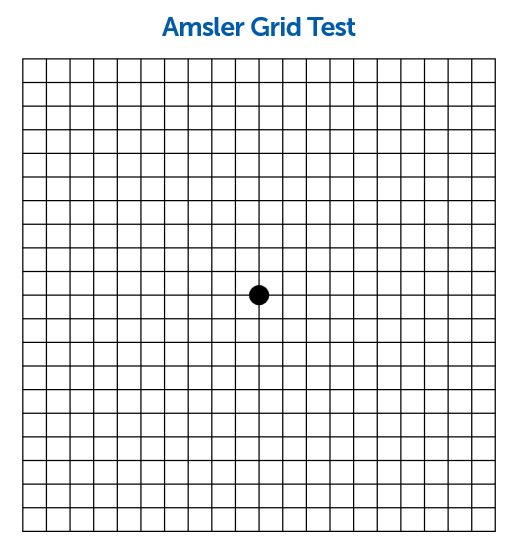
Amsler Grid
The Amsler grid looks like typical graph paper. To a normal eye, each of the lines on the graph should be sharp, in focus, and with no areas of distortion. The grid is be used by testing each individual eye and if any areas of waviness, darkness or blurriness develop, a patient should be immediately examined by an ophthalmologist. The Amsler grid is an excellent option but does have some limitations. These include incorrectly using the grid and not using the grid frequently enough. One of the greatest concerns of the Amsler grid is by the time symptoms are noticed on the grid, there has already been significant vision loss.
- Wear your reading glasses, if you normally use them and sit about 14 inches away from the screen.
- Cover the left eye.
- With the right eye, focus on the dark dot in the center of the grid.
- While looking at this dot, you still should be aware of the lines of the grid. Notice if any of the lines are distorted or broken or if there are blurred areas.
- Now, cover the right eye and repeat the test.
- If you notice any blurred, wavy or missing lines, contact your ophthalmologist as soon as possible.
ForeseeHome Monitoring Device
The ForeseeHome Monitor® from Notal Vision® is the first FDA-cleared device for patients with dry AMD to monitor the disease at home. It is now a Medicare-covered service for patients enrolled in Medicare across the U.S., and who meet the eligibility criteria for dry AMD at high risk for converting to wet AMD. The device is designed to be used daily and takes approximately 3 minutes per eye. When used daily, the ForeseeHome Monitor detects changes before a patient would notice, and allows the doctor to monitor the vision for any changes that take place between regularly scheduled exams. In a clinical trial that involved over 1500 participants, the device demonstrated that 87-94% of users maintained 20/40 vision or better at the time of wet AMD detection, compared to only 62% of those who used conventional methods such as the Amsler grid. Vision at this level is significant because vision that is better than 20/40 allows patients to maintain their usual level of independence.
They are able to read, maintain their driving license and continue to function at a very high level. A separate monitoring center processes each test and your prescribing doctor receives a monthly report. If there is a deviation from the usual testing, an alert would be triggered that would inform the prescribing doctor of a change that may be suggestive of wet macular degeneration. The prescribing doctor would then do a complete eye examination to assess if there has been a change to wet AMD. To learn more, please visit: http://www.foreseehome.com.

Macular degeneration continues to have promising treatments in the pipeline to preserve and improve vision. Home monitoring and addressing reversible or controllable risk factors remain as important as ever. If you or a family member have macular degeneration, your next eye exam is not too soon to start asking questions about your options and risk.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Dry AMD
- Prevention
- Risk Factors