In light of positive results from a BrightFocus-funded Phase I study of an innovative glaucoma therapy involving eye implants, a Phase 2 clinical trial of this exciting potential treatment is currently enrolling patients.
The study is testing an implant that delivers a steady stream of growth factors, called ciliary neurotrophic factor, to protect against damage to the optic nerve. Optic nerve damage is a hallmark of glaucoma, a major cause of blindness worldwide. The implant could prevent further vision loss by preserving retinal ganglion cells, which make up the optic nerve.
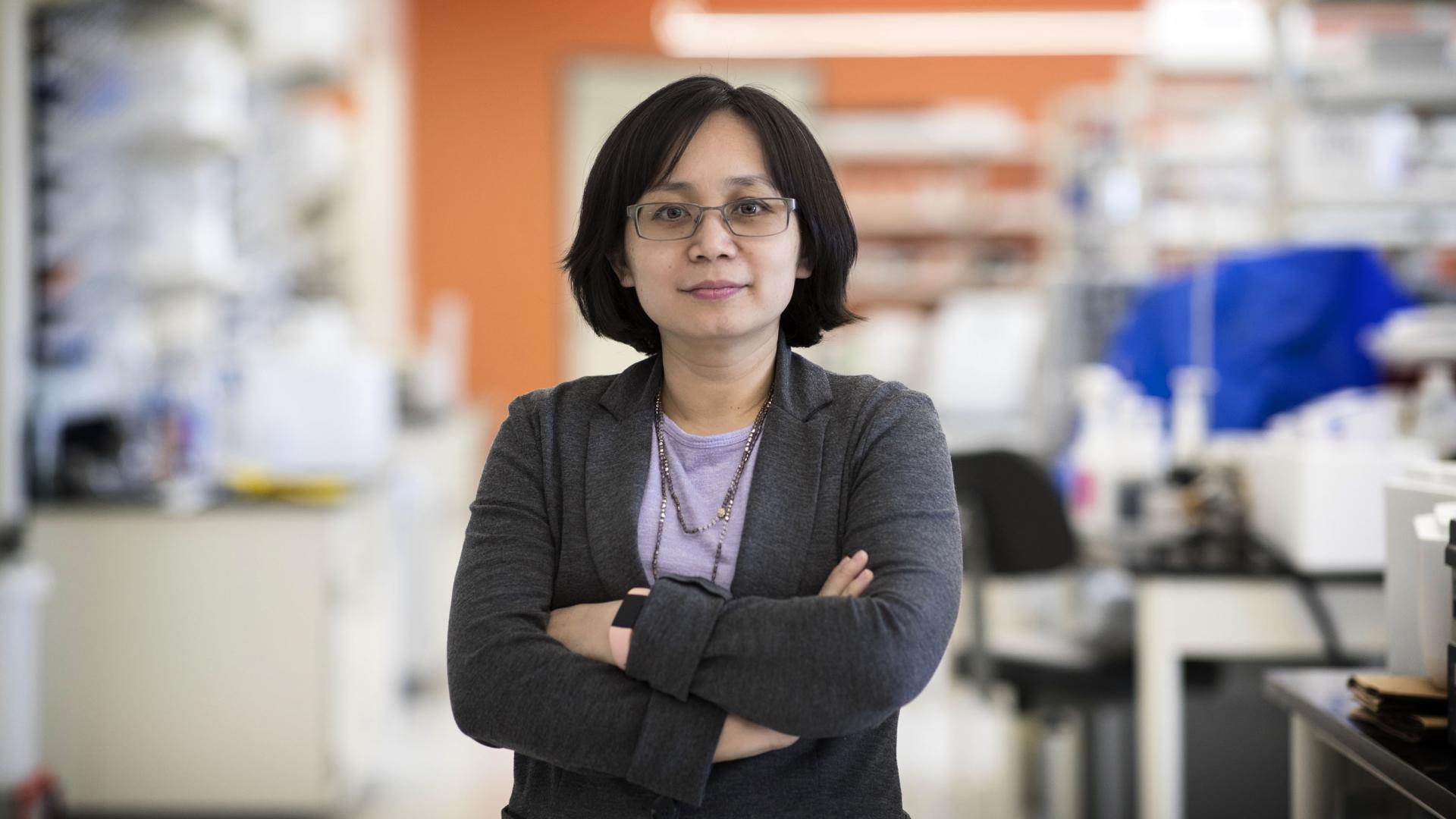
Leading the study is BrightFocus grantee Jeffrey Goldberg, MD, PhD, chair of ophthalmology at Stanford University. He specializes in optic nerve protection and regeneration and has received support from BrightFocus’ National Glaucoma Research program.
Safety shown in Phase I trial
The Phase I trial tested the safety of the implant in 11 people who were diagnosed with primary open-angle glaucoma, the most common form of the disease. One eye of each patient was assigned as the study (implant) eye, and the second served as a control. Patients were followed for 18 months.
The implant was found to be safe and well tolerated. There were no serious side effects and none of the patients needed to have the implant removed.
In addition, eyes with the implant showed improvement over the non-treated eyes, paving the way for the Phase 2 trial in a larger population with glaucoma. Learn more about the Phase 2 trial, which is being funded in part by BrightFocus.
In the development of a new drug or treatment, a Phase 2 clinical trial tests whether the treatment is safe in humans and researchers also gather information on its effectiveness. Learn more about clinical trials.
How the procedure works
The experimental treatment, labeled NT-501, is a type of encapsulated cell therapy. It has been previously tested in age-related macular degeneration and in an inherited form of retinal degeneration known as retinitis pigmentosa and has recently completed Phase 3 trials in another eye disease, macular telangiectasia.
In glaucoma, the goal of the NT-501 implant is to protect vision by preserving retinal ganglion cells (RGCs). Existing approved glaucoma therapies are directed at treating the intraocular pressure regulated at the front of the eye. The work of Dr. Goldberg and his team involves an innovative approach aimed at the RGCs at the back of the eye.
RGCs receive visual signals from the photoreceptors in the eye and send them over long fibers, called axons, that extend via the optic nerve to the brain. In glaucoma, damage from increased intraocular pressure damages the axons in the optic nerve and kills RGCs, resulting in vision loss. The body cannot repair or replace RGCs.
The NT-501 is a capsule filled with cells designed to secrete growth factors that is implanted into the eye to protect RGCs. The procedure involves making a small incision through the sclera (the white part of the eye), inserting the implant, and securing it with a suture.
The Phase 2 study is expected to be completed by the end of 2024, and includes patients implanted with either one or two implants per treated eye—the first such trial to examine the safety and efficacy of two implants to test increasing the dose. The primary goal of the study is to measure changes in vision, and secondary goals are to evaluate the health of the optic nerve through several means.
Questions for Dr. Goldberg
With currently approved glaucoma therapies focusing on treating the intraocular pressure at the front of the eye, what led you to focus on the neuroprotection of the retinal ganglion cells (RGCs) in the back of the eye instead?
Maintaining vision in glaucoma is too often not achieved with current approaches that focus on lowering eye pressure. Whether using eye drops, lasers, or even surgeries, in some patients the vision or visual field continues to get worse. We need new approaches that directly treat the retinal ganglion cells and/or the optic nerve. My research in the lab over the past two decades has focused on understanding the retinal ganglion cells degeneration and failure to regenerate, and discovering the molecules and treatments that can successfully intervene. In the clinic, I’ve been focused on moving promising therapies from the lab into human trials that have a chance of benefiting patients.
Do you expect the results from the Phase 2 trial to show that vision was maintained in glaucoma patients, or do you expect the results to show actual improvement in vision?
Either of these would be amazing steps forward in our field. If we can further slow or stop the degeneration that occurs in glaucoma, maintaining vision, we call that “neuroprotection.” If we can actually improve vision, for example if the treatment takes sick retinal ganglion cells and makes them healthier again, we call that “neuroenhancement.” Our trial is designed to detect either of these, should they occur.
Since this is a sham controlled trial (an inactive procedure designed to mimic the procedure being studied in the clinical trial), some patients will not be implanted with NT-501. If early results are promising, would those patients be offered the investigational treatment?
Actually, we designed this trial with all of our patients in mind. Patients are randomized to single implant, double implant, or sham implantation (nothing gets put inside the eye), but they are not told until one year later which group they are in. This improves the rigor of the trial, by keeping the patient masked to which group they are in. However, all patients are told one year later, and the patients who were in the sham group are offered an option to now get the real implant. So every patient has a chance at the real thing.
How can people with primary open-angle glaucoma enroll in the trial?
Anyone can reach out regarding our clinical trials by visiting this website. There is a form patients can fill out as well as contact information.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Through its flagship research programs — Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research— the Foundation has awarded nearly $300 million in groundbreaking research funding over the past 51 years and shares the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.