Cataracts and Glaucoma: What You Should Know in 2024
Featuring:
Aakriti Garg Shukla, MD
Leonard A. Lauder Assistant Professor of Ophthalmology at Columbia University Medical Center


Aakriti Garg Shukla, MD
Leonard A. Lauder Assistant Professor of Ophthalmology at Columbia University Medical Center

Does glaucoma cause cataracts? Can cataracts and glaucoma be treated at the same time? Learn more during a conversation with guest expert Aakriti Garg Shukla, MD, who will discuss the relationship between cataracts and glaucoma.
Dr. Shukla is the Leonard A. Lauder Assistant Professor of Ophthalmology at Columbia University Medical Center. She received her medical degree at Columbia University College of Physicians & Surgeons, where she completed her ophthalmology residency and served as Chief Resident. She pursued further glaucoma subspecialty training at the Wilmer Eye Institute at Johns Hopkins University in Baltimore, MD. She was an assistant professor of ophthalmology at the Wills Eye Hospital prior to her relocation to New York.
Dr. Shukla has published over 70 peer-reviewed articles and book chapters and has been invited to speak nationally and internationally on patient care and research. She serves on the Ophthalmology and Ophthalmology Glaucoma editorial board, the World Glaucoma Association Associate Advisory Board, the AGS Glaucoma Screening Task Force, the AAO Sustainability Task Force, and the ASCRS Young Eye Surgeons Clinical Committee. Her research interests include structure-function relationships in glaucoma, optimization of surgical outcomes, and sustainability in ophthalmology. She is passionate about trainee education in the clinic and operating room and is committed to excellent clinical care.
MS. KACI BAEZ: Hello, and welcome to today’s BrightFocus Glaucoma Chat. My name is Kaci Baez, VP of Integrated Marketing and Communications at BrightFocus, and I’m so happy you’re here today to chat with us about Cataracts and Glaucoma: What You Should Know in 2024. Our Glaucoma Chats are a monthly program, in partnership with the American Glaucoma Society, designed to provide people with glaucoma and the family and friends who support them with information straight from experts. BrightFocus is committed to investing in bold research worldwide that generates novel approaches, diagnostic tools, and life-enhancing treatments that serve all populations in the fight against age-related brain and vision diseases. Today, we’re excited to introduce guest expert, Dr. Aakriti Shukla. Dr. Shukla is the Leonard A. Lauder Assistant Professor of Ophthalmology at Columbia University Medical Center. Dr. Shukla has published over 70 peer-reviewed articles and book chapters and has been invited to speak nationally and internationally on patient care and research. She serves on many advisory boards, and her research interests include structure–function relationships in glaucoma, optimization of surgical outcomes, and sustainability in ophthalmology. She is passionate about trainee education in the clinic and operating room and is committed to excellent clinical care. Welcome, Dr. Shukla.
DR. AAKRITI SHUKLA: Thank you so much for having me.
MS. KACI BAEZ: Thanks for joining us on this Valentine’s Day as we show our eyes some love. So, today we’ll just dive right in and talk about glaucoma and cataracts, and just starting off with a foundation of: What is a cataract?
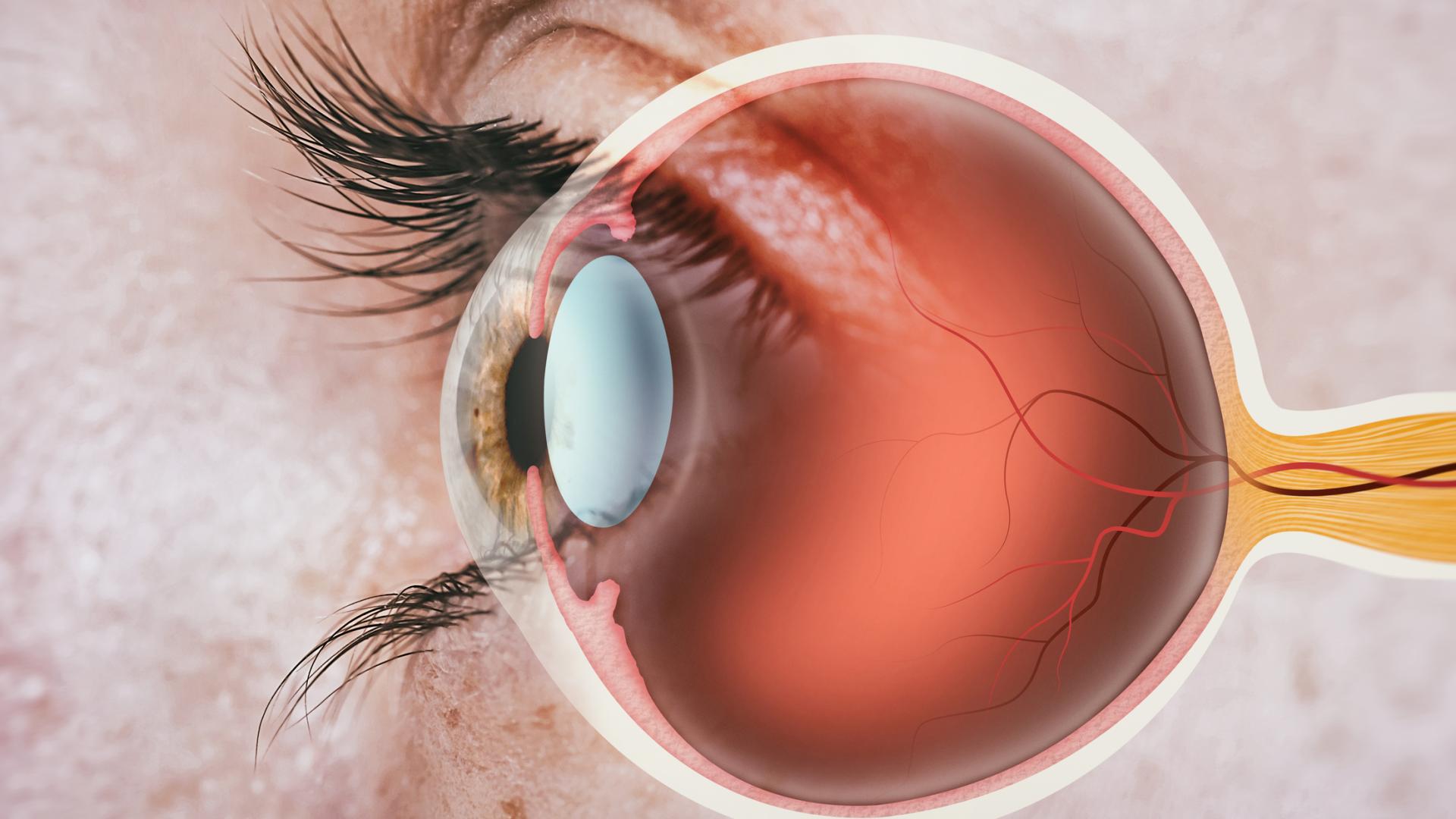
DR. AAKRITI SHUKLA: Great question. What is a cataract? A cataract is clouding of the natural lens of the eye. This lens lies between the iris, right behind the pupil—the very center of the eye. The lens adjusts its shape and thickness to focus the light rays that enter through the cornea and through the pupil onto the retina. And the clouding of the lens can lead to vision problems by preventing light from passing clearly through the lens, causing blurred or distorted vision. A cataract is a common condition that’s associated with aging, but can also occur due to other reasons, like injury, the use of certain medications, or certain medical conditions. I guess we should also talk about what glaucoma is—see if we can quickly define that, too. Glaucoma is a number of different eye diseases that are characterized by specific patterns of optic nerve damage that’s visible when one views the optic nerve—just by looking at the optic nerve—and also, when one tests the function of the optic nerve—so, visual fields are another way to kind of test for glaucoma. In glaucoma, lowering the eye pressure usually slows the progression of disease, so it prevents someone from getting worse glaucoma. And although the lowering of the eye pressure is important in preventing the worsening of glaucoma, the eye pressure can really be high or normal or even low, and one can still have glaucoma.
MS. KACI BAEZ: Thanks for explaining what glaucoma is. It’s important to understand that it’s not just one disease, but a series of diseases. And cataracts versus glaucoma—I think there’s differences in being able to reverse glaucoma versus cataracts. So, do cataracts cause glaucoma? And what are the symptoms of cataracts in comparison to glaucoma?
DR. AAKRITI SHUKLA: Good question. Cataracts themselves usually do not cause glaucoma. However, both conditions can coexist in the same individual. Sometimes, people with very advanced cataracts have an increased risk of having elevated eye pressure, and this can lead to the increasing risk of developing glaucoma. A large lens or a more spherically shaped lens can sometimes also cloud the anterior chamber angle, which is where the natural drain of the eye is located, and removing the lens in these cases can help lessen the risk for particular types of glaucoma in which the angle of the eye becomes very narrow or closed. They are, however, distinct conditions. Cataracts—I like to say that, if we all live long enough, then we’ll all get cataracts. Glaucoma, however, does not affect the entire population in the way that the cataracts do with time.
The symptoms of cataracts versus the symptoms of glaucoma: There is some overlap in symptoms, but they’re fairly different. Symptoms of cataracts include blurry or cloudy vision, difficulty seeing at nighttime, a fading of colors—people tell me they can no longer match socks as well or the movies just don’t seem as bright to them. People also complain of glare; sensitivity to light; seeing halos around lights, especially when driving or looking at streetlights. Glaucoma, on the other hand, often early on, has no symptoms. People do over time describe experiencing some glare. They can also see that maybe they have some peripheral or maybe even central vision loss or areas of blurring, areas where the images don’t seem as crisp. In the later stages of glaucoma, and I guess the final stages of glaucoma, the eye can completely lose vision.
And what’s very important that distinguishes the two conditions also is that glaucoma leads to irreversible vision loss, so anything one loses from the glaucoma, we cannot bring that back. It’s all about preventing the vision loss due to optic nerve damage in glaucoma. Cataracts, however, are completely reversible, so when one decides to get cataract surgery, any vision that’s lost from the cataract really should come back after that surgery. So in general, when patients have cataracts, for the most part, I leave it up to them when they want to get the cataract surgery. However, with glaucoma, sometimes it really requires educating the patient and talking to them about the condition and really explaining that we’re trying to prevent vision loss in this case and kind of creating that sort of understanding with the patient. And sometimes having them undergo surgery even when they don’t necessarily have symptoms, just to try to prevent those symptoms from developing over time if we think that glaucoma will progress without that sort of treatment.
MS. KACI BAEZ: Does glaucoma actually cause cataracts?
DR. AAKRITI SHUKLA: That’s a good question. Glaucoma does not directly cause cataracts. They are separate eye conditions, but a person can have glaucoma and cataracts simultaneously. They have some of the same risk factors—the main one being age. And another example is if one has a history of eye trauma or if one chronically uses steroid medications, both of these situations can increase the risk of cataract development earlier in life and can also increase the risk of glaucoma.
MS. KACI BAEZ: That’s so fascinating. And can a person be more at risk for glaucoma versus their risk for cataracts? Understanding that they are different diseases, and age is a factor for both, but can a person just naturally be more at risk for one versus the other?
DR. AAKRITI SHUKLA: That’s a good question. I guess maybe first I’ll speak about cataracts. Like we were saying, everyone, if we are lucky to live long enough, we’re all going to develop cataracts over time. There are some families in which cataracts show up earlier; sometimes babies are born with cataracts, and they need cataract surgery very early on in their life to allow them to develop vision in their eyes. And then, there are some people who get cataracts in their 30s and 40s, requiring cataract surgery. But I would say the majority of people who are getting cataract surgery are at least in their late 50s and beyond. So, aging is really the primary risk factor for cataracts. Other risk factors also include diabetes, smoking, prolonged exposure to sunlight, and certain medications. Glaucoma, however, affects anywhere from 2 to 6 percent of the population, a much lower percentage than cataract. And the risk factors for glaucoma include age, especially those over the age of 50; a family history of glaucoma—if one has a first-degree relative with glaucoma, they have a nine times greater risk of the disease, and most people are unaware they have this greater risk with that family history; certain types of ancestries—so, African American ancestry or Asian ancestry can often predispose one to glaucoma. That’s just a more common condition in those groups. Those of Hispanic ethnicity are also at higher risk of developing glaucoma. And people who have diabetes are at higher risk of developing glaucoma. In general, we recommend that everyone 40 years or older should have a comprehensive eye exam performed every 1 to 2 years to pick up these conditions because, especially as we were talking about glaucoma, it’s totally asymptomatic in the beginning, so it really requires the physician picking this up on eye exam. Patients really can’t tell in the beginning that this is something that’s affecting their eyes.
MS. KACI BAEZ: Okay. Thank you. And I think many people don’t realize that cataracts and glaucoma can both occur even as early as birth, so understanding your history and your risk is so important, as you mentioned. You touched on the eye exam, so what exactly happens during an eye exam for cataracts, and how is this different from an eye exam for glaucoma?
DR. AAKRITI SHUKLA: Sure. Good question. A complete eye exam is required for both cataract and glaucoma diagnoses. And it’s important to rule out other conditions that can lead to vision loss. This generally involves going in person to see the doctor. They’ll check your visual acuity—so, that means reading off the eye chart that we’re all pretty familiar with. They’ll check your intraocular pressure—so, that’s the pressure inside your eye, which is different from blood pressure. They’ll check your visual fields and assess the reactivity of your pupil to see how well the eye reacts and the iris constricts to light. A microscope called a slit lamp will be used to assess the front of the eye, which includes the cornea, the iris, the lens, or the cataract, as well as the back of the eye, which includes the retina and optic nerve. And—especially when we’re assessing glaucoma, but really for everyone—everyone deserves one gonioscopy exam. In this exam, a special mirror is used to assess the angle of the eye—that’s where the natural drain of the eye is located. And if the angle of the eye is deemed to be open, your ophthalmologist will likely dilate the eye to better assess the cataract and evaluate the posterior segment—that’s where the retina and the optic nerve are. And if there’s any suspicion of glaucoma or retinal disease, your doctor will perform a special scan of your optic nerve and retina, called optical coherence tomography. This test takes a picture of your optic nerve and retina and really uses light waves to visualize microscopic abnormalities that may be present. This test can help us determine if the earliest signs of glaucoma are present. You’ll also have the thickness of your cornea measured, because this can be a risk factor for glaucoma, as well. If there is a suspicion of glaucoma, they’ll also check your peripheral or side vision, as this is most commonly affected first. Of course, some patients can have central loss prior to their peripheral visual field involvement, but all of this really needs to be tested using automated perimetry, which is kind of a standardized way of checking one’s visual field.
If your doctor is planning on doing cataract surgery or if they see a visually significant cataract, and they’re discussing it with you, they will obtain a biometry test that helps measure the front and back of the eye, and it also takes some measurements of the lens itself. They may also obtain a map of the cornea to see how the cornea is shaped. They’ll measure your refraction or what type of glasses you’re currently using. They’ll also, importantly, have a conversation with you about your preferences about what sort of activities you like to do, and are you someone who wishes to see at distance without glasses and wear reading glasses for up close, or are you someone who prefers to be able to read without glasses, and you really don’t mind glasses for driving? Once your doctor has all of this information, they’ll help you choose an intraocular lens—or an artificial lens—that best fits your eye’s anatomy and your own preferences, and then that’ll be the lens that they’ll put in during the cataract surgery.
MS. KACI BAEZ: Okay. So, you mentioned cataract surgery. What are all of the treatment options for cataracts, and can cataracts and glaucoma be treated at the same time?
DR. AAKRITI SHUKLA: Great question. The early symptoms of cataracts, like a little bit of blur or changing refraction, can be helped with just getting a new pair of glasses. But eventually, one reaches the point where glasses are not really helping, and the glare and the dimness and maybe the lack of color contrast is something that’s bothersome enough, and then you go down the surgery route. The only real way to fix cataracts is performing cataract surgery. That’s the only way to treat the cataract. And the surgery involves removing the cloudy lens and replacing it with a clear intraocular lens, which is an artificial lens. Let’s talk a little bit briefly about the surgery. This is the same-day outpatient surgery. You get there about an hour before surgery; surgery itself can take anywhere from 10 to 50 minutes based on the complexity of your cataract—it may take even longer if other procedures are required—and then the patient goes home typically about an hour after surgery. Several decades ago, patients used to stay in the hospital for cataract surgery for several days, but this is definitely not the case anymore.
Let’s talk a little bit about the surgical day. You arrive at the surgical facility about an hour or two before surgery. When you get there, they’ll have you change into a gown, you’ll get an IV put in your arm, you’ll review some paperwork, and then they’ll dilate your eye, and you’ll go into the operating room. During the surgery, you’ll receive twilight anesthesia. It’s a similar type of anesthesia as one would get for a colonoscopy, so you can hear some sounds, see some lights, but you really shouldn’t feel any pain, and you shouldn’t feel anxious about the situation. During the surgery, as I mentioned, we remove the lens, the cataract, and put in a new, clear intraocular lens. And then once the surgery is all wrapped up, then you go into the postoperative recovery area, where you wake up from anesthesia pretty much instantly and then are on your way home about 30 minutes or so later.
You asked whether we can treat cataract and glaucoma at the same time. This is becoming increasingly more common. There are different types of surgeries for glaucoma. There’s a whole category of surgery called minimally invasive glaucoma surgery. These have become more popular in the last 10 to 12 years or so, and these typically involve either the placement of a tiny stent in the eye, and that stent goes into the natural drain of the eye, or it involves a procedure called goniotomy, in which we create an opening in the natural drain of the eye, and that opening helps us bypass resistance in the natural drain of the eye that we think is present in people with glaucoma. There are a number of other minimally invasive glaucoma surgeries in the pipeline. I would say those are probably the two most common ones.
There are also bigger surgeries for glaucoma, including trabeculectomy and a tube shunt. And both of these surgeries actually involve creating a brand-new drain for the eye. In trabeculectomy, we create a drain using your eye’s natural tissues, and in the tube shunt, we actually place an implant onto the eye that acts like the new drain for the eye. And these surgeries can be done at the same time as cataract surgery. One of the advantages of doing that is that it’s really one surgical procedure for the patient, so it’s one instance of anesthesia and tends to be more convenient in that way. It’s also just one recovery process, so it’s all done at the same time. Your doctor will be the best person to assess, first of all, whether you need cataract surgery, then if you do have glaucoma, whether you need minimally invasive glaucoma surgery along with the cataract surgery, or one of the conventional surgeries, including trabeculectomy and tube shunt. But there are plenty of options, and it’s a nice opportunity to try to limit some of the eye drops that you may be on. I would say that sometimes the recovery takes a little bit longer if one is to get a glaucoma procedure along with cataract surgery, so that’s something we can talk about a little bit more, but that is just one small consideration. But many times, it really is worth it to do these additional procedures to get the glaucoma under control at the same time as doing the cataract surgery.
MS. KACI BAEZ: So, how safe would cataract surgery be for glaucoma patients? Are there risks or adverse effects on patients with glaucoma when it comes to cataract surgery?
DR. AAKRITI SHUKLA: Great question. Cataract surgery is generally safe for all glaucoma patients. The main risk of cataract surgery includes infection inside the eye, bleeding inside the eye, changes to the eye pressure, needing to go back to the operating room to do a second procedure, or needing to go back if the entire lens was not able to be removed from the eye. The risk of all of these outcomes happening is really very, very low—it’s less than 1 percent. If your eye has a particular type of anatomy, let’s say you are someone who’s extremely nearsighted and there is some risk of retinal detachment in everyone who’s getting cataract surgery, but if your anatomy is very different from average—such as if you’re very nearsighted—then your risk of retinal detachment may be a little bit higher. Everyone’s individual risk is different, but the overall risk is extremely low, and the risk for glaucoma patients doesn’t really differ from the risk of the cataract surgery for the average person in a big way.
You’ll want to be sure that your surgeon knows how to manage glaucoma during the postoperative period, because there can be some temporary increases in pressure associated with some of the postoperative eye drops or even some of the solutions that we use during the surgery. For these reasons, your doctor may need to watch you more closely than other patients who undergo cataract surgery and do not have glaucoma. As mentioned, your recovery, if you have glaucoma, and especially if you undergo glaucoma procedure along with cataract surgery, may take longer than if you’re getting cataract surgery alone. But then, of course, you’re getting the benefits of the glaucoma procedure, as well, and your sight will be maintained, perhaps in a superior way than if you were to just get cataract surgery alone.
MS. KACI BAEZ: Okay, thank you. Will cataract surgery lower eye pressure, and should one have cataract surgery instead of glaucoma surgery?
DR. AAKRITI SHUKLA: That’s a good question. Cataract surgery has been demonstrated to have a modest effect on eye pressure. And in many cases, it has been shown to lower eye pressure anywhere from 2 millimeters of mercury to 10 millimeters of mercury, and some people having less or more of an effect there. This is especially the case in eyes with angle closure glaucoma. In these eyes, the front of the eye is smaller and kind of more crowded than the average eye, so removing the cataract, which tends to be pretty bulky, and putting in an intraocular lens—the artificial lens, which actually is very thin—can open up a lot of space in the anterior chamber, and then that can help lower the pressure. So, in some folks who have angle closure glaucoma, doing the cataract surgery, even doing it alone as a first step, may be what your physician chooses to do instead of doing cataract surgery plus glaucoma surgery as a first step. It’s really so individual for every patient, but I would say if you’re going to do cataract surgery instead of glaucoma surgery, and for angle closure eyes, that’s something I would certainly consider. But if somebody has very advanced glaucoma and has high pressures, and clearly showing signs of damage and maybe even progression, then probably you need more than just cataract surgery alone. You probably need a combined cataract and glaucoma procedure.
MS. KACI BAEZ: Thank you. Always important to get a personalized plan and guidance with your doctor, but it’s so great to have so many options. When it comes to implants, what are the different types of lens implants, and which lens should someone with glaucoma get?
DR. AAKRITI SHUKLA: Great question. So, there are a variety of different types of intraocular lenses, including monofocal lenses, multifocal lenses, and toric lenses, and they’re each designed to address specific visual needs. In general, we do not recommend multifocal lenses for patients with glaucoma because the advantage of multifocal lenses is that they can theoretically help you see at distance and up close without the use of glasses. So, it’s kind of like the vision that we all have when we’re young, where we’re not reaching for reading glasses or anything like that and we have good vision at a distance and up close. However, these lenses can lower your overall contrast sensitivity, making your overall vision more dim, and in patients with glaucoma and other eye conditions that are already reducing their vision, multifocal lenses are not recommended in that case. Toric lenses are an option for certain people who have certain types of astigmatism that affect the cornea, that change the curvature of the cornea, and these are assigned options. So, if there’s a patient with glaucoma who has significant corneal astigmatism and it’s deemed to be regular corneal astigmatism and I can’t find other corneal problems, toric lenses are a fine option for folks with glaucoma and astigmatism who do not need conventional glaucoma surgery at the same time as cataract surgery or anytime in the near future. And the reason is that conventional glaucoma surgery can actually change the corneal curvature and would change the type of toric lens someone would need, so we don’t recommend the toric lens procedure if other surgeries are planned. And then monofocal lenses are the most common type of lenses that are put in the eye, and they’re a safe choice for everyone.
MS. KACI BAEZ: Okay, great. And so the lenses, are they different for closed angle versus open angle glaucoma?
DR. AAKRITI SHUKLA: Great question. Lens choices shouldn’t differ too much for people with closed angle or open angle glaucoma. Your surgeon may identify other risks, such as not having support in the capsular bag, which is where the artificial lens will fit after cataract surgery. So, they may end up choosing a particular type of lens, such as a three-piece lens, to have the lens in the eye in these cases. And if they don’t find enough support in the capsular bag, they may avoid something like a toric lens, which can rotate and move, and if that happens, you end up needing an even bigger glasses prescription than you may have had before. So, in general, there really shouldn’t be any difference in lens choices between closed angle versus open angle glaucoma. But there are so many other considerations about the eye’s anatomy the surgeon takes into account when choosing the type of lens.
MS. KACI BAEZ: Okay. Thank you. That’s so helpful. And our listeners do have a lot of questions around this topic, and one of the questions we received is: Should people with glaucoma receive steroids during cataract surgery or use steroids after the surgery? And how often are glaucoma patients steroid responders versus people without glaucoma?
DR. AAKRITI SHUKLA: This is a great question. After cataract surgery, the eye generally responds very favorably to cataract surgery. The average person does very well, but everybody needs some sort of anti-inflammatory eye drop after cataract surgery. And I would say, for most surgeons, the drops of choice are a steroid eye drop, so almost everyone’s going to be on some sort of steroid after cataract surgery. Generally, we start with something like prednisolone four times a day. Some people might need it more frequently, and then we taper it off after cataract surgery over the course of about a month or so. Over time, now, these kind of depo steroids have become more common, and the advantage of these depo steroids is that patients don’t have to use drops as often after surgery or may not have to use drops at all. These are fine options, but in the setting of glaucoma, I would hesitate to use these on my patients because of this risk of steroid response. The nice thing about drops is if I start to see that, “Okay, I’m having my patients using the steroid drops. The pressure is starting to go up,” then I know that I can always decrease the frequency of the steroid drop and manage their pressure that way. A steroid depo is something that’s going to be sitting in the eye, that’s going to be acting, and I have no way to titrate the effect of the steroid after surgery. So, personally, I would recommend definitely using steroid drops and probably avoiding the steroid depo.
So, how do the steroids work? The steroids can alter the microstructure of the trabecular mesh work, which is the natural drain of the eye. It can influence the turnover of the substances that live there, which can increase the resistance to outflow and can increase the eye pressure. What percentage of the population has steroid response? It’s hard to know exactly how many, but it’s been estimated that about 30 percent of people show a moderate increase in pressure after using these steroid eye drops, and about 5 percent of people are highly responsive to these steroid eye drops in which they have high IOP elevation—like, more than 10 millimeters of mercury—once they start using steroid eye drops. So, there is a proportion of the population that’s going to be very sensitive. I watch my patients very carefully when I start them on these types of medications, just knowing that it’s possible, and it is more common amongst people who have glaucoma to have this response to the steroids compared to people who don’t have glaucoma. So, I’m certainly more aware in my patient population, and I look out for this, and that’s really the reason why I would avoid the longer-acting depo steroid.
MS. KACI BAEZ: Okay. Thank you. That is so helpful. We have an additional listener question, and it’s: Can cataracts cause a blind spot area to be reported on visual field test?
DR. AAKRITI SHUKLA: Good question. Cataracts can definitely affect one’s vision, and that’s why we choose to do cataract surgery, to improve people’s vision and quality of life. They can also show up in the visual field in certain ways. Generally, in glaucoma, we’re looking for focal defects in the visual field. Cataracts can lead to an overall more generalized depression of the visual field. So, it’s interesting, of course, get baseline visual fields on everyone, but sometimes it’s fun to kind of check the visual field a month or two after the person’s had cataract surgery. And many times, there’s some improvement in the visual field after the cataract surgery, because that kind of generalized depression has lifted once the cataract has been removed. So, there can be some areas that are kind of faded or have more of a defect because of cataracts in the visual field.
MS. KACI BAEZ: Okay, great. Thank you. And just thinking about the cataract surgery again, you mentioned taking drops for a certain number of weeks, but how long does it take generally to recover from cataract surgery, particularly if you have glaucoma?
DR. AAKRITI SHUKLA: I usually tell people that it will take about a month to be fully recovered. And for a certain proportion of people, it’s going to take longer than a month. And I would say probably in the majority of people, it takes less than a month, but I ask people to expect at least a month for recovery. Generally, I tell people the day after surgery, “You may feel that the vision is a lot better, you may feel that it’s worse, you may feel it’s the same. It’s hard to predict that, but a week out after surgery, you’ll probably feel that the vision has improved, and then a month out you will feel a pretty significant improvement.” But like I said, there is a proportion of people who will take even longer to improve and to stabilize.
MS. KACI BAEZ: And do you have any tips on how to have a successful recovery from cataract surgery if you have glaucoma?
DR. AAKRITI SHUKLA: Good question. Number one, of course, following your doctor’s guidance and instructions to the “T” would be helpful. There are going to be a lot of things that change, so if you’re someone who has cataracts and glaucoma, you’re most likely going to be on some sort of eye drop for glaucoma before surgery. It’s very important to know after the surgery exactly how the drops are changing because, more than likely, your surgeon’s going to start you on a steroid drop, and then an antibiotic drop, and then you need to ask them, “Well, what should I do now with my glaucoma drops? Should I continue them? Should I take them off?” And a lot of that’s going to be dependent on whether you have just a cataract surgery alone or whether you had cataract plus a glaucoma surgery. Your surgeon will be able to tell you that. Generally, you’ll be asked to use a clear plastic shield to cover the eye when you’re sleeping, and that’s really to prevent the eye from hitting your pillow or from accidentally rubbing the. Usually for about a week or so, you’re told to restrict your activities, not lift anything heavier than 10 pounds, not bend over or doing activities that would really strain your body. I tell people it’s absolutely fine to use your eyes for anything you’d like—you can read, watch TV, etc. And those are kind of my standard instructions. I also tell people no eye makeup, don’t get soap in your eyes for a few days.
I also tell people, importantly, everyday things should be the same, or they should get a little bit better. If anything is getting worse, that’s really not normal, and our office needs to be alerted right away. The risk of infection after cataract surgery is rare, but if it happens; it’s very serious and needs to be treated right away. So, really, following your doctor’s instructions, I think, is the best way to go about doing things. Something additional that you could consider is using some more artificial tear drops to lubricate the eye to kind of optimize the ocular surface to help speed up recovery. If you are using artificial tear drops, I’d recommend waiting about 30 minutes between the medicated drops and artificial tear drops because you don’t want the artificial tear drops to dilute the medicated drops.
MS. KACI BAEZ: Great. Thank you. That’s really helpful. And our listeners have another question, and it’s: What pressure range indicates that MIG surgery should accompany cataract removal?
DR. AAKRITI SHUKLA: Interesting question. It’s really so different for everyone, and the answer to this question depends on, number one, how much glaucoma damage the person has. So, if you have very advanced glaucoma and your pressures are 20, that really might be too high, given you have advanced glaucoma, and so then you probably do need combined glaucoma and cataract surgery. If you have no evidence of glaucoma at all, and you just have pressures that are above whatever target pressure that your doctor has set for you, it’s possible that the MIGS option is kind of an optional thing. But a lot of it depends on your level of glaucoma damage—how many eye drops you’re using, how well you’re able to tolerate those eye drops, what your rate of progression is, and not only how much damage do you have, but how quickly is it getting worse? A number of different considerations, so there’s really no cutoff in the range of pressures that tells me this person definitely needs MIGS or not. But for most people who are on a drug, they are looking for opportunities to get off that drug. And the MIGS procedure or other glaucoma procedures do give you those opportunities. So, I usually offer it to most patients, if possible, if they’re already on a glaucoma eye drop or if they have significant findings of glaucoma when I examine their optic nerve or have them do a visual field.
MS. KACI BAEZ: Okay, great. Thank you. And our last question from our listeners: If you have retinal vein occlusion, can you still have surgery for glaucoma and cataracts?
DR. AAKRITI SHUKLA: Good question. Retinal vein occlusion and glaucoma have been found to be somewhat comorbid in that they are kind of associated to occur together. They don’t always occur together, of course, but there is some association between those two conditions. And certainly, if you have a history of retinal vein occlusion and you have uncontrolled eye pressures, then certainly you can have glaucoma surgery. And cataract surgery, like we talked about, everyone in their lifetime, if they live long enough, will need cataract surgery, so that’s fine to do in the setting of retinal vein occlusion, as well. Whenever I do these surgeries in the setting of any retinal disease—and specifically, retinal vein occlusion—I work very closely with a retina specialist because it’s possible that you may need an injection in your eye of anti-VEGF, which is the vascular endothelial growth factor medicine that can help reduce swelling before the surgery or help prevent swelling from developing in the eye after the surgery. So generally, if you have a history of retinal vein occlusion, I would make sure that your retina specialist knows that I’m planning on doing cataract surgery, and your retina specialist may choose to do one of these injections or pretreat you with a certain kind of nonsteroidal anti-inflammatory eye drop prior to the cataract surgery to prevent the chance of swelling or other problems related to the retinal vein occlusion occurring after cataract surgery.
MS. KACI BAEZ: Thank you, Dr. Shukla. That’s so valuable for our listeners to know. These topics are so complex, and surgery can generate a lot of complex feelings and questions. It’s always helpful to be prepared with expert information. Is there anything you’d like to share with our listeners regarding glaucoma and cataracts? Any parting tips on the subject that maybe we haven’t touched on?
DR. AAKRITI SHUKLA: I think your questions have really been excellent and comprehensive. The biggest thing I would say is I think it’s important for the listeners to know that they really should form a connection with their glaucoma specialist. This is someone that they’re going to know for a very long time, as glaucoma is a chronic disease and it’s sort of a silent disease that the glaucoma specialist has to help translate for the patients by evaluating all the scans and testing that we do. It’s important for the glaucoma specialist to really help the patient understand what all of these things mean and what the significance of the condition is. So, make sure that you take time to really get to know your glaucoma specialist and that you feel comfortable with the person that you’re seeing because that person is going to be an important person who helps navigate the field of ophthalmology and helps navigate a condition that can be pretty anxiety provoking otherwise. So, that would be my main advice to the listeners out there. Make sure you find the glaucoma specialist you love.
MS. KACI BAEZ: Excellent. Thank you so much, Dr. Shukla, for all the important information that you shared with us today. That wraps up our questions and thank you to our listeners so much for joining us today for our Glaucoma Chat. We sincerely hope that you found it valuable. Next month on Wednesday, March 13, we will dive into Building Connection and Community: Take Charge of Your Glaucoma Diagnosis, and we hope that you can join us then. And until then, thank you again for joining us, and that concludes today’s BrightFocus Glaucoma Chat.
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.

In this chat, Dr. Poonam Misra addresses some of the most common questions listeners have shared over the past year—from treatment options and lifestyle considerations to the latest educational resources.

Dr. Astrid Werner explains what causes dry eye, how to recognize the symptoms, and effective treatment options—including preservative-free drops, artificial tears, and eyelid care routines.

Meet Richard, a loyal donor to BrightFocus' National Glaucoma Research and Macular Degeneration Research programs.
Join us for a fascinating conversation with Dr. Lucy Q. Shen as we explore cutting-edge research into restoring vision loss from glaucoma.
Support Groundbreaking Glaucoma Research
Your support helps fund critical research that could prevent vision loss, provide valuable information to the public, and cure this sight-stealing disease.
Donate Today