Pigmentary Glaucoma and Pigment Dispersion Syndrome
Written By: BrightFocus Editorial Staff
Written By: BrightFocus Editorial Staff
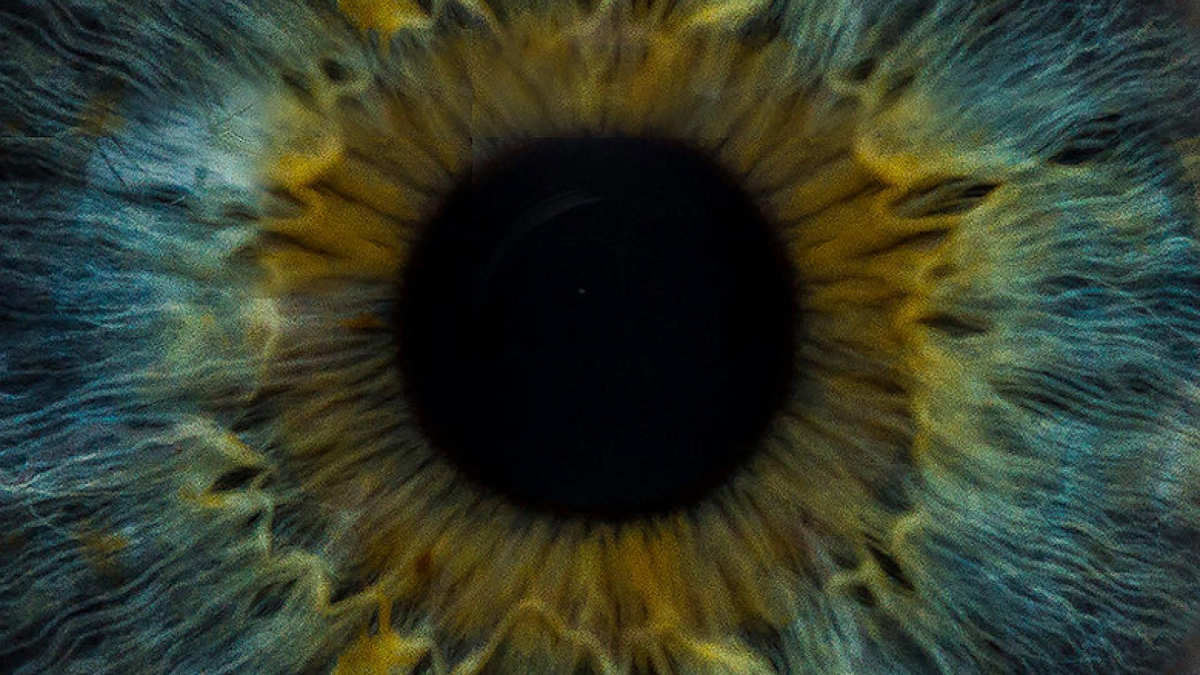
Learn about a form of glaucoma that results from pigment granules that flake off from the iris (the colored part of the eye) and clog the eye’s drainage system, thereby resulting in high eye pressure, and subsequent damage to the optic nerve.
Pigment dispersion syndrome (PDS) is diagnosed when there is pigment released in the eye that results in deposits on structures in the front of the eye. These pigment deposits can clog the drainage system of the eye, thereby resulting in high eye pressure.
Pigmentary glaucoma (PG) is diagnosed when the pigment dispersion syndrome results in damage to the optic nerve. For the purposes of this article, we will discuss pigmentary glaucoma, but please understand that some patients may have pigment dispersion but not yet have glaucoma.
This form of glaucoma can be an insidious disease without symptoms, and thus it is especially concerning that it is most commonly diagnosed in the third or fourth decade of life (younger than the most common form of the disease: open-angle glaucoma).
Pigmentary glaucoma tends to occur in males more than females, in patients with nearsightedness (myopia), and at a younger age (20-40 years old). Family history is sometimes positive for pigmentary glaucoma, although certainly one can have the disease without a family history.
It is thought that due to the anatomy of the eye, there is some contact between the iris (the part of your eye that forms the pupil), and the lens and its associated structures, so that there may be chafing or rubbing during normal activities such as focusing the eyes in order to read.
There is also a possibility that vigorous exercise can cause increased pigment release. Thus some patients are advised to take medications to lower eye pressure prior to exercise or avoid exercise altogether. If you have PDS and are concerned about this, please speak to your ophthalmologist before starting or stopping any exercise program.
The pigment that is released can deposit on various structures in the front of the eye, and eventually can clog the drainage system. Some people’s drainage systems do not have a problem handling this extra pigment, and these patients do not develop glaucoma. Other people’s drainage systems cannot handle this extra “load,” and eye pressure builds up, eventually leading to the development of glaucoma. It is estimated that 30-35 percent of patients with pigment dispersion syndrome develop high eye pressure and/or glaucoma.
Typically many patients do not have symptoms, especially early in the disease process. When pigmentary glaucoma advances, a patient may notice difficulty with side vision, just as one would experience in open-angle glaucoma. Rarely, patients may complain of sporadic episodes of haloes or blurry vision. In order to be diagnosed with pigmentary glaucoma, your ophthalmologist needs to do a thorough examination of your eyes, including an examination of your drainage angle.
Patients with pigment dispersion or pigmentary glaucoma have more pigment than usual in the drainage angle. They may also have pigment on the inner lining of the cornea and thinning of the iris from where the iris chafing occurs and pigment is released. A detailed examination of the back of the eye is also needed in order to assess if there is any optic nerve damage. You may undergo imaging of the optic nerve as well as formal field of vision testing to check for side vision problems.
The treatment of pigmentary glaucoma involves lowering eye pressure by using medications, laser, or surgery, which is similar to the treatment options for open-angle glaucoma.
The usual medications that lower eye pressure for open-angle glaucoma are also used for pigmentary glaucoma. Some advocate using an older glaucoma medication called pilocarpine because it sometimes can alter the anatomy of the eye so that there is less chafing and pigment dispersion. However, pilocarpine has many side effects, including an increased risk of retinal detachment, for which patients with nearsightedness (common in pigmentary glaucoma patients) already have a slightly increased risk.
There are differing opinions as to the usefulness of a laser procedure to make a small hole in the iris, which is usually used to prevent or treat angle-closure glaucoma. In the case of pigmentary glaucoma, the purpose of the hole is to help shift the anatomy in the eye so that there is less chafing or rubbing of the iris and thus less pigment dispersion.
A different type of laser (laser trabeculoplasty) can also be used to improve drainage and lower pressure, which can be very effective in pigmentary glaucoma because of the increased pigment in the drainage angle. Finally, surgical options such as trabeculectomy or tube shunt surgery can also be used to treat more aggressive forms of pigmentary glaucoma.
Since pigmentary glaucoma can have no symptoms, and because it typically occurs at a younger age, this form of glaucoma is often underdiagnosed. However, if identified early and treated appropriately, patients often do well, and blindness from this form of glaucoma is relatively rare. In some cases there is the possibility of regression of the pigment dispersion over time, and sometimes there is even a return to “normal” eye pressures. As always, with any type of glaucoma, regular follow-up examinations with your ophthalmologist are critical to the preservation of sight.
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
Support Groundbreaking Glaucoma Research
Your support helps fund critical research that could prevent vision loss, provide valuable information to the public, and cure this sight-stealing disease.
Donate Today