This article explores the risks and benefits of laser peripheral iridotomy (LPI), when it is used, and what to expect if you have this procedure.
Types of Laser Surgery for Glaucoma
There are different types of laser surgery depending on the type of glaucoma. For example, one type of laser surgery (laser trabeculoplasty) is often used in open-angle glaucoma when medications are unlikely to work, do not work, or produce intolerable side effects. In some patients, laser trabeculoplasty may be the first mode of therapy if eye drops are not practical or likely to be used improperly.
On the other hand, in angle-closure glaucoma or in patients at risk for this condition, another type of laser surgery (laser iridotomy) is the preferred method of treatment right from the beginning.
Narrow-Angle Glaucoma Diagnosis
Using a special mirrored lens in a procedure called gonioscopy, your ophthalmologist can check your eye’s drainage system. When the angle is open, your ophthalmologist can see most, if not all, of your drainage system. On the other hand, when the angle is narrow, your ophthalmologist can only see portions of the drainage angle, and in acute angle-closure glaucoma, none of the drainage angle is visible. Gonioscopy is the most common way your ophthalmologist can diagnose narrow angles, and you may be diagnosed as a primary angle-closure “suspect.”
What Causes Narrow Angles?
You may have narrow angles because of certain anatomical conditions, such as having a shorter eye than the average person, being hyperopic (far-sighted), or having a growing cataract that gradually narrows the angle over time. You may also have a closed angle because of inflammatory conditions, such as uveitis, or vascular conditions, such as diabetes, that gradually cause what is termed “secondary angle closure” over time.
Video: What Are Narrow Angles?
Acute Angle-Closure Glaucoma: A Medical Emergency
If you are a primary angle-closure “suspect,” you may be at risk for a potentially very serious condition called acute angle-closure glaucoma. Often these acute angle-closure attacks take place when the pupil dilates, for example, in a dark movie theater. In this situation, the pressure may slowly build up in the back part of the eye due to the narrowness of the angle (when the pupil dilates, the drainage structures can become partially obstructed in someone with narrow angles). This pressure build-up gradually increases and causes the iris to push forward and the angle to narrow even further, eventually blocking off most or all drainage of fluid from the eye. When this happens, the eye pressure increases dramatically. The cornea may become cloudy due to the increased pressure, the eye may become quite red, and vision will be decreased. The increased eye pressure can also cause pain, sometimes so severe that it leads to nausea and vomiting. Finally, there is irreversible damage to the optic nerve, the part of the eye that transmits light and visual information to the brain.
Treatment for Acute Angle-Closure Glaucoma
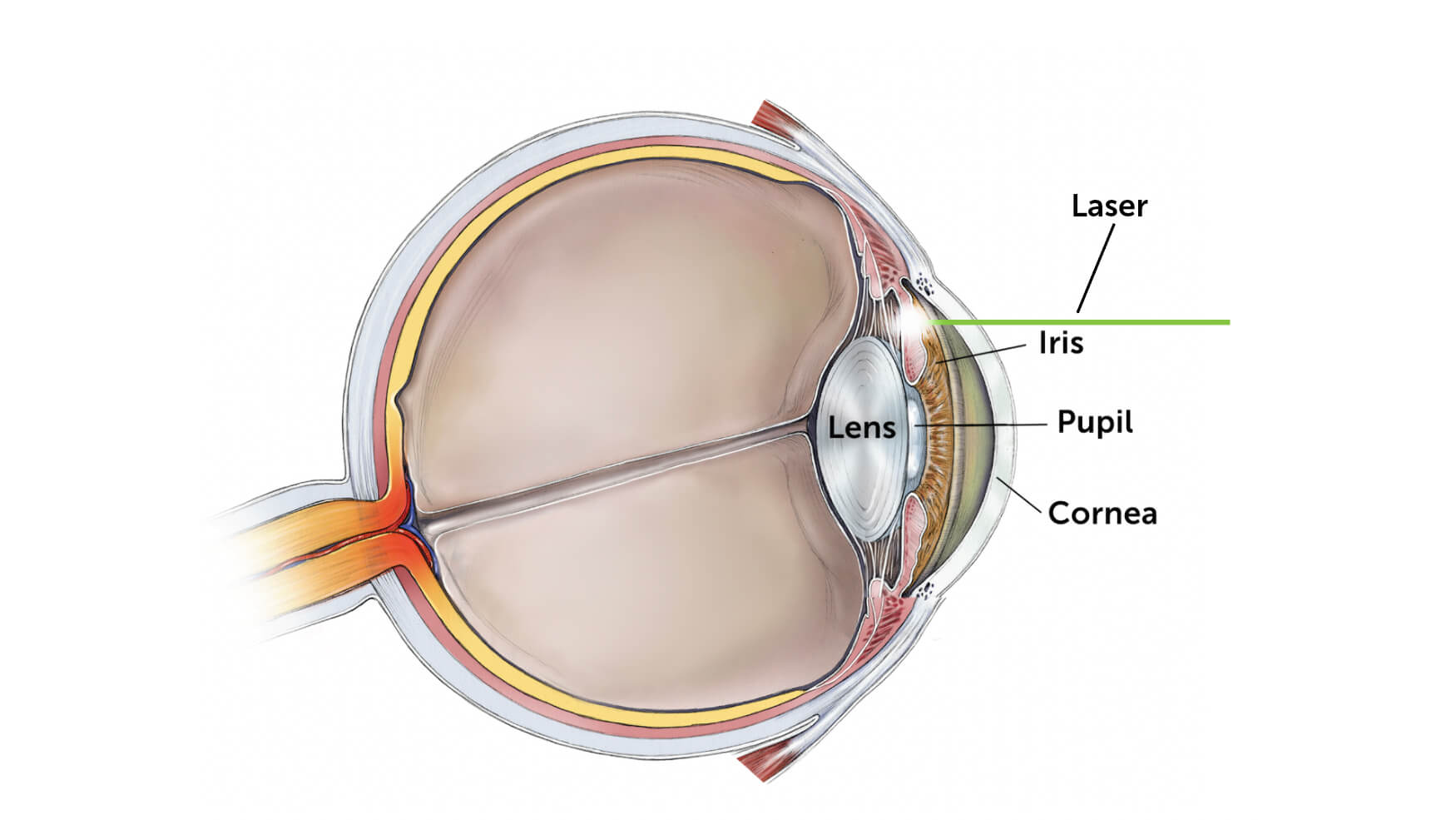
The treatment is to lower eye pressure using eye drops and potentially oral medications, but the definitive treatment at the time of the glaucoma attack is to perform a laser iridotomy. In this procedure, a tiny hole is placed in the iris to allow the iris to fall away from the drainage area inside the eye. You can think of the hole as an escape valve so that the pressure in the front of the eye equalizes the pressure in the back of the eye.
Video: What is Acute Angle-Closure Glaucoma?
Iridotomy to Prevent Angle-Closure “Suspects”
Laser peripheral iridotomy is the same procedure used to preventively treat primary angle-closure suspects, or patients with narrow angles that are at risk for an angle-closure attack. Although there are some criteria that ophthalmologists use to determine whether a patient with narrow angles is at high enough risk to warrant this preventive procedure, there is no way to predict whether any given individual will actually go on to have an angle-closure attack if left untreated.
Preventing Angle-Closure Glaucoma with Iridotomy
Although not all patients with narrow angles go on to develop angle-closure glaucoma, laser iridotomy is often performed as a preventive measure because of its relatively low risk compared to the potentially serious consequences of angle-closure glaucoma. If an iridotomy is performed early enough in the process, it may be curative. Some patients still require drops or supplemental laser treatment, however. Practically speaking, laser surgery has the advantage of being an in-office procedure with a very low risk for serious complications. Finally, sometimes there are other reasons that might lean in favor of performing a laser iridotomy, including the need for frequent dilated eye exams in diabetic patients. Dilation causes the iris to bunch up in the angle and can precipitate an angle closure attack. There are also many oral medications that can cause pupil dilation or other changes within the eye that can result in an angle closure glaucoma attack.
What Happens During Laser Peripheral Iridotomy?
Here’s what you can expect from your LPI surgery:
- First, the eye is anesthetized. This is done using the same types of eye drops used for measuring eye pressure. Some additional preparatory eye drops may also be used.
- Next, the patient is set up in front of the laser, which looks like the typical examination microscope.
- Then a contact lens is temporarily placed on the eye.
- The laser beam is aimed and multiple laser “shots” are placed into the iris. (Laser surgery is not painful although the patient may feel a “pop” in the eye or an occasional pin-prick type sensation.)
- At the end of the laser peripheral iridotomy surgery, the contact lens is removed and the eye rinsed out. Another eye drop may then be given.
- Your eye pressure will be checked 30-60 minutes after the procedure is completed.
- After your iridotomy, you may notice some blurry vision, mild discomfort, or a foreign body sensation in your eye. These symptoms are usually transient and are gone within a few hours to a few days. You may also be given some anti-inflammatory medication to use for a few days to a week to prevent any significant inflammation.
Video: Laser Peripheral Iridotomy
Risks and Benefits of Laser Peripheral Iridotomy
Is Laser Iridotomy Safe?
It is understandably difficult for patients who see an eye care provider during a routine visit to be told that they have narrow angles requiring a laser procedure. Furthermore, an internet search about laser iridotomy is sure to uncover some scary stories of patients with unpleasant experiences. However, laser iridotomy has low risk of side effects and is a very safe procedure that prevents a potentially devastating eye condition.
Nonetheless, it is important to understand the risks and benefits of laser peripheral iridotomy in order to make an informed decision about whether to undergo the procedure. As outlined above, the benefit of this procedure is that it may prevent you from having a potentially visually devastating angle-closure attack. Although the risk of progressing to an angle-closure attack is unknown, the possible outcome is so impactful that it is worth considering the benefit of laser peripheral iridotomy.
What Are the Risks?
- In terms of risks, common complications include a little bleeding from the iris (almost always transient). If you are taking a blood thinner such as aspirin, Plavix (clopidogrel), Xarelto (rivaroxaban), Eliquis (apixaban), or Coumadin (warfarin), make sure you tell the doctor. Depending on your ophthalmologist’s preference, it may be advisable to discontinue the blood thinner a week or so before the procedure. If bleeding does occur, some pressure may be placed on your eye with a contact lens and your vision may be a little blurry for a few hours to a day.
- Mild light sensitivity and a scratchy feeling on the surface of the eye are also common for 24-72 hours after the procedure.
- Rarely, the patient may experience an extra “ghost image” or “halo” through the tiny opening in the iris. This may be annoying for a while but almost all of the few patients who develop this complication eventually get used to it and are not bothered by it.
- Lastly, it is not uncommon to have a mild eye pressure elevation after the hole through the iris is made since iris pigment is released during the procedure. Therefore, your eye pressure will be checked 30-60 minutes after the iridotomy, and in cases of mild eye pressure elevation some eye drops may be used to lower the pressure.
Alternatives to Peripheral Iridotomy Surgery
Alternatives to laser iridotomy include a surgical iridectomy in which an incision is made in the eye to remove a portion of the iris. Surgical iridectomy has more significant risks than laser iridotomy and is rarely used anymore. The other alternative is to do nothing, which runs the risk of an acute attack of angle-closure glaucoma that may be difficult to control and cause serious visual damage. There is also now evidence that removing any cataract by performing a cataract extraction surgery is an appropriate treatment for angle-closure glaucoma and even primary angle-closure suspects.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Through its flagship research programs — Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research— the Foundation has awarded nearly $300 million in groundbreaking research funding over the past 51 years and shares the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Glaucoma Surgery