This article addresses the use of lasers to lower eye pressure as a treatment for glaucoma, and explains what to expect during the procedure.
Glaucoma is a chronic, progressive deterioration of the optic nerve, the bundle of nerve fibers at the back of the eye that carry visual messages from the retina to the brain. Glaucoma is often caused or worsened by pressure inside the eye(intraocular pressure) that is too high for the continued health of the optic nerve.
Managing Eye Pressure
Glaucoma treatment is aimed primarily at reducing the intraocular pressure to a safe level that will prevent or at least slow the nerve damage. Eye pressure is the major risk factor in the development of optic nerve damage from glaucoma and is the only factor that doctors can currently treat. In most cases, treatment consists of eye drops or laser surgery that either improves the drainage of fluid or reduces the formation of fluid inside the eye. Either medications or laser surgery can be used as “first-line” treatment. Typically patients will have a preference for one or the other and we will discuss that in greater detail below.
Two Forms of Surgery
Surgical techniques include delicate laser or microscopic incisional methods. Generally, laser methods are tried before incisional surgery, although sometimes laser surgery is not appropriate for the condition or is not likely to bring the eye pressure low enough. It is also important to understand that there are many different types of lasers used in ophthalmology that range in their purpose and procedure.
Incisional Methods
The microscopic incisional methods include trabeculectomy with mitomycin C or 5-fluorouracil application, glaucoma drainage device (or tube) implantation, cyclophotocoagulation, and ExPRESS microshunt implantation. In addition, there are newer, minimally invasive glaucoma surgeries such as the Trabectome, iStent, Kahook dual blade, Cypass*, or Xen implant that are combined with cataract surgery. These procedures are likely safer than traditional surgeries, but often do not lower the eye pressure enough for moderate to advanced glaucoma. Each surgery has its own special uses, advantages and disadvantages; the decision for which surgery to perform should involve a discussion between you and your ophthalmologist.
* In 2018, the manufacturer of the CyPass® micro-stent to treat glaucoma decided to voluntarily withdraw it from the market. Learn why the manufacturer took this step, and what you should do if you have already had the CyPass micro-stent procedure.
Laser Options
Laser surgery is often used in open-angle glaucoma (the most common form of this eye disease) when medications do not work, are unlikely to work, or produce intolerable side effects. In some patients, laser surgery may be the first mode of therapy if eye drops are not practical or are unlikely to be used properly. For example, some patients do not want to use daily eye drops, either because they are difficult to instill in a consistent manner, have intolerable side effects, or are costly. For these patients, laser therapy may be their first choice. A patient and their doctor can weigh the risks, benefits, and side effects of laser treatment versus medications, and determine the best treatment with which to start.
-
Laser Trabeculoplasty
Laser trabeculoplasty is used in several types of open-angle glaucoma. It is used less commonly in angle-closure glaucoma after iridotomy has opened the drainage system or in mixed-mechanism glaucoma where both the open and closed angle forms of glaucoma co-exist.
-
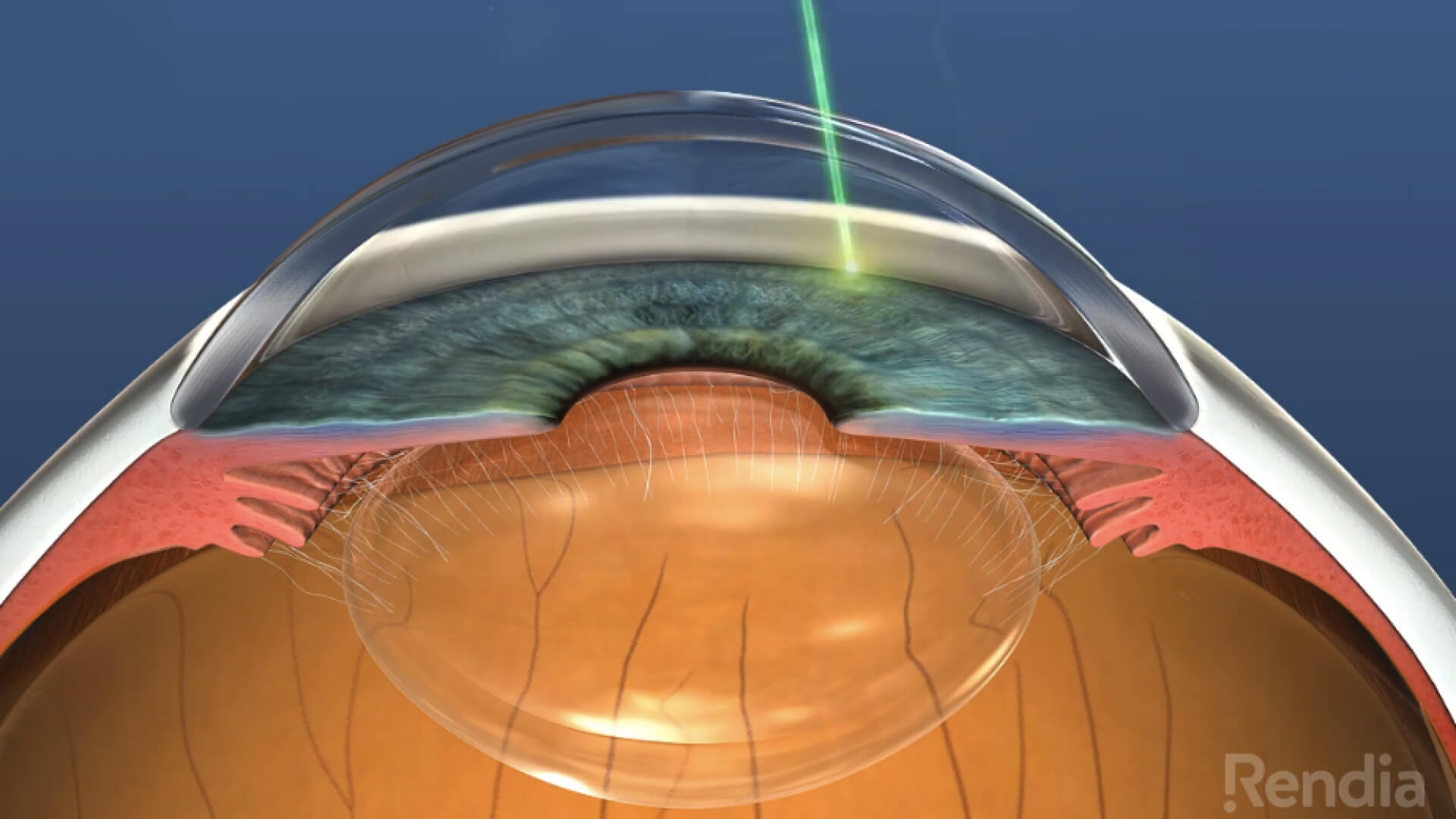
Selective Laser Trabeculoplasty (SLT)
Selective laser trabeculoplasty (SLT) is a fairly recent advance. The laser used in this technique was especially developed for this job. The laser does not burn tissue, but rather vaporizes the pigment that may be affecting the cells in the drainage system and improves the drainage of fluid from the eye. Since there are no burns, this laser technique can be repeated. The laser beam is aimed directly at the drainage system through a mirrored contact lens with the intent of improving the drainage of fluid out of the eye and thus lowering the pressure. While trabeculoplasty does not work in all patients, it is often used because of its relative safety. The success rate is about 60-70 percent in lowering the eye pressure by 20 percent. For many patients, this is an ideal procedure as it can either eliminate the need for eye drops or reduce the number of eye drops, but it is important to remember that the laser procedure is not a “cure.” The effect of the laser can wear off over time, although it can be repeated.
View a Video on SLT
What to Expect During the Procedure
Laser surgery has the advantage of being an in-office procedure with a very low risk for serious complications. Laser surgery does not require hospitalization or any change in daily activities. In most laser surgery, the eye is anesthetized with the same eye drops used for measuring the eye pressure. After the patient is set up in front of the laser, which looks like the typical examination microscope, a mirrored contact lens is temporarily placed on the eye. Laser surgery is not painful; however, the patient may feel an occasional pinprick type sensation. After the procedure is over, the contact lens will be removed and the surface of the eye is rinsed. Another eye drop may be given and the eye pressure will be checked again to ensure that it is not elevated. Sometimes the pressure rises transiently and rarely it may rise for a long period of time necessitating surgical intervention (which would have been necessary anyway if the laser option were not available).
Summary
Laser surgery to lower eye pressure can be very effective and safe, and has a definite place in the ophthalmologist’s toolbox. In order to decide whether laser surgery is the correct treatment for you, a detailed conversation with your ophthalmologist will help you in making that decision.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Eye Health
- Treatments









