This article explores the risks, benefits, and potential complications of tube shunt surgery as a treatment for glaucoma.
Many people with glaucoma are able to successfully control their eye pressures—and prevent vision loss—for years and even decades through the use of prescribed medications. However, if eye drops and other medications prove ineffective, or if the patient can’t tolerate side effects from medications, then the doctor may recommend surgery.
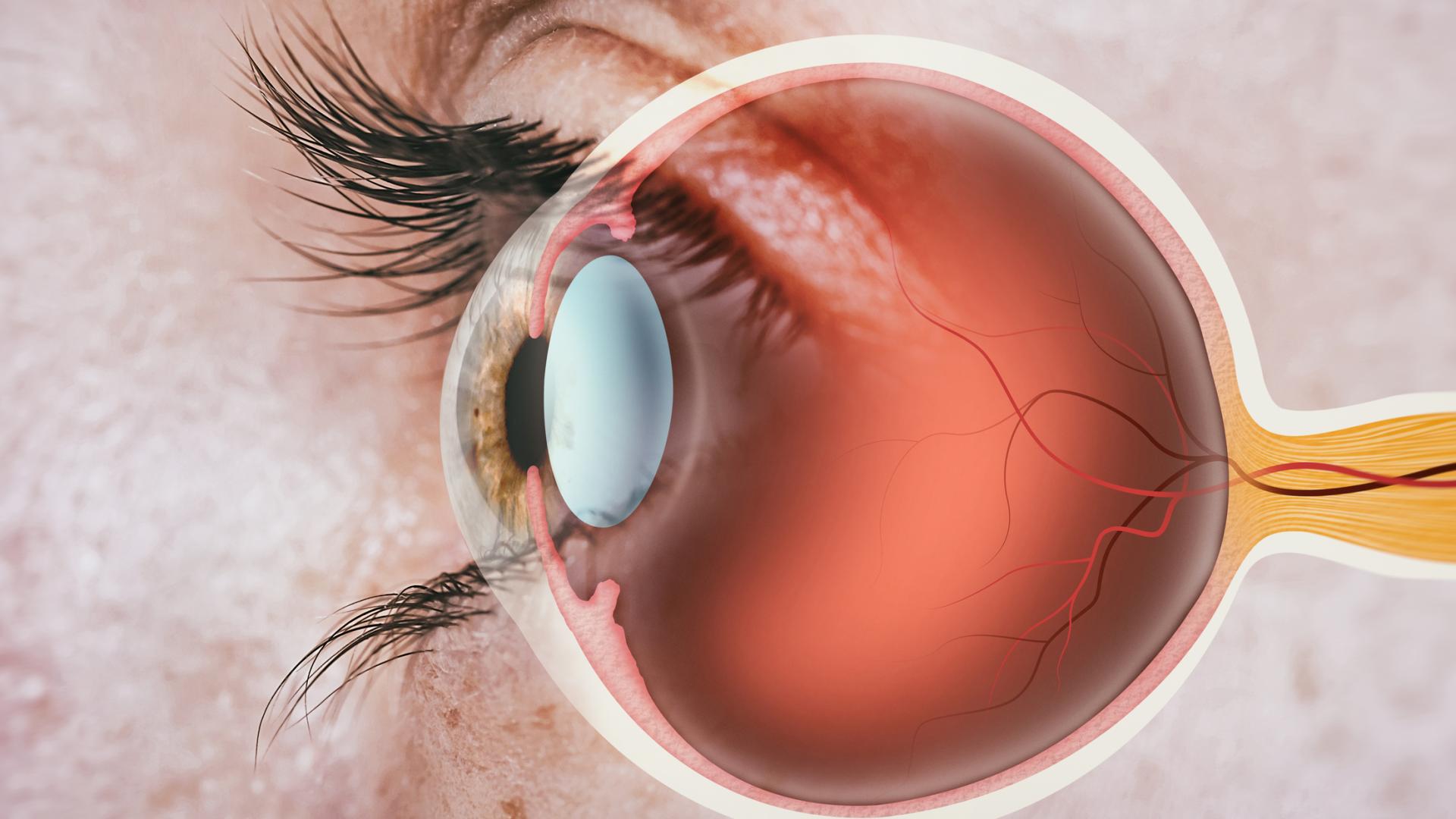
One type of incisional glaucoma surgery uses a tube shunt, which is a flexible glaucoma drainage device that is implanted in the eye to divert aqueous humor (the fluid inside the eye) from the inside of the eye to an external reservoir.
The Ahmed Glaucoma Valve is a commonly used type of glaucoma drainage implant made of silicone or polypropylene, a material that won’t break down in the body. The entire implant is covered with the eye’s own external covering.
The Ahmed shunt itself is shaped like a miniature computer mouse with a tube at the end of it. The tube portion enters the front of the eye, or anterior chamber, while the rest of the implant sits on the surface of the eyeball underneath the conjunctiva and is covered by the eyelid. The fluid that collects is then absorbed by the eye’s own veins and transported out of the eye cavity.
The Ahmed valve implant procedure is done as outpatient surgery.
Video: Tube Shunts for Glaucoma
Who Is a Candidate for Glaucoma Tube Shunt Surgery?
Traditionally, tube shunts were used to control eye pressure in patients in whom traditional eye surgery to relieve fluid pressure had previously failed, or in patients who have had previous surgeries or trauma that caused substantial scarring of the conjunctiva. Tube shunts have also been successful in controlling eye pressure in other types of glaucoma, such as glaucoma associated with uveitis or inflammation, neovascular glaucoma (associated with diabetes or other vascular eye diseases), pediatric glaucoma, traumatic glaucoma, and others was conducted in patients who had previous surgery, including, trabeculectomy and/or cataract surgery. Those results showed that after five years, tube shunt surgery had a higher success rate compared to trabeculectomy, with similar reductions in eye pressure and the need for supplemental glaucoma medications.
In recent years, some surgeons are using tube shunts or glaucoma drainage devices as first-line surgery, and forgoing standard trabeculectomy as the first surgery. Generally, trabeculectomy is thought to reduce the eye pressure to a greater degree than tube shunt surgery, but there are greater risks. To weigh these factors, there is currently an ongoing trial comparing tube shunt versus trabeculectomy in patients who have had no prior ocular surgery (PTVT Study: Primary Tube vs. Trabeculectomy Study; stay tuned for results). The tube shunt is covered by Medicare and most insurance plans.
Tube Shunts and Valves
A “valve” is one type of tube shunt that could be implanted during your tube shunt surgery. There are several types of tube shunts available and typically the tube shunt that is chosen is based on your specific situation and the surgeon’s preference. The Ahmed Glaucoma Valve is the most commonly used type of shunt.
The valve function of a glaucoma drainage device limits the flow of eye fluid in one direction, which puts a theoretical limit to how low the eye pressure can drop. However, in many patients, supplemental glaucoma medications such as eye drops are still required after an Ahmed valve is implanted to keep eye pressure within a normal range.
Sometimes the tube shunt is not attached to a valve (e.g., the Baerveldt or Molteno shunts). In this case, some scarring has to take place initially before the tube opens, otherwise the eye pressure will be too low. The tube opens when a special suture that the surgeon has used to tie off the tube dissolves over time, or another type of suture that the surgeon will remove approximately 4-6 weeks after surgery in the office. The risk of the eye pressure falling too low, while rare, is somewhat higher with these devices than with the Ahmed valve, but non-valved shunts sometimes work better for attaining a lower eye pressure.
Comparisons: Ahmed Device vs Baerveldt Shunt
Because the various tube shunts have different sizes, features, and surgical techniques associated with them, the decision of which tube shunt to have implanted depends on your particular situation and your surgeon’s preference.
There have been two multicenter, randomized, clinical trials examining the Ahmed (valved) device versus the Baerveldt (non-valved) shunt. The Ahmed Baerveldt Comparison (ABC) study demonstrated that both types of tube shunts had similar surgical success at 5 years. The Baerveldt resulted in greater eye pressure lowering but there were more early and serious complications associated with the Baerveldt as compared to the Ahmed valve.
The Ahmed Versus Baerveldt (AVB) study, an international, multicenter, randomized trial, demonstrated that both devices were effective in lowering eye pressure but the Baerveldt group had lower failure rate and required fewer glaucoma medications with lower eye pressures after five years. However, the Baerveldt group had more serious complications associated with the eye pressure being too low (similar to the findings in the ABC study).
Benefits, Risks, and Possible Complications
The vast majority of tube shunt procedures are successful and prevent the progression to blindness that can occur with glaucoma. Nonetheless, it is important for you to understand the risks and benefits before electing a tube shunt surgery. Any of the complications described below can occur even with the best surgical techniques. The vast majority of complications are short-lived or can be fixed, while serious complications are much more rare.
- Infection
As a precaution, ophthalmologists give antibiotics during and after the surgery in addition to practicing sterile technique. However, on very rare occasions, infection inside the eye occurs anyway. This can be a very serious problem and may threaten vision. With tube shunt surgery, infection can occur months to years after the actual operation, sometimes requiring shunt removal. Your eye doctor can talk with you about how to prevent late infections like this. Have your ophthalmologist look at your eye immediately if there is any sign of infection.
- Failure of the Tube Shunt
Any tube shunt procedure may fail, with time, due to the natural healing tendencies of the eye. Your body is reacting to a “foreign object,” the tube shunt, and scarring around the plate is not uncommon. As a result, you may need to resume glaucoma medications down the road, or even soon after surgery. In addition, sometimes a repeat surgery is required. On the flip side, sometimes tube shunts, especially the non-valved implants, can result in too low of an eye pressure, or hypotony. Some patients with hypotony will have vision impairment. Sometimes the tube will have to be revised or removed if hypotony persists.
- Uncommon or Rare Complications
Uncommon or rare complications include bleeding inside the eye; fluid buildup behind the retina (choroidal detachment, which is not the same as retinal detachment); double vision with some types of implants; tube-related complications; and infection, as mentioned above. Bleeding inside the eye can be a very serious complication; for this reason, some surgeons will ask you to stop all blood thinner medications for at least one week before the surgery. Make sure you ask your general doctor if this is acceptable. If not, a discussion should occur between the ophthalmologist and the general doctor before the surgery.
Also, despite successful surgery, your vision may become worse from continuing degenerative changes in the eye. Cataracts may be accelerated by any of these operations. Fortunately, cataracts are relatively easy to fix surgically.
About BrightFocus Foundation
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
- Glaucoma Surgery