Childhood Glaucoma
Featuring
Javaneh Abbasian, MD
Chief of Ophthalmology, Jesse Brown VA Medical Center; Clinical Associate Professor of Ophthalmology, University of Illinois at Chicago


Javaneh Abbasian, MD
Chief of Ophthalmology, Jesse Brown VA Medical Center; Clinical Associate Professor of Ophthalmology, University of Illinois at Chicago

Learn about the different types of childhood glaucoma, including primary congenital, infantile, and juvenile glaucoma. Guest expert Dr. Javaneh Abassian explained the role of genetics and associated systemic diseases, trauma-induced cases, and diagnosis and treatment.
Dr. Abbasian is a board-certified ophthalmologist who is dual fellowship trained in both pediatric ophthalmology and adult glaucoma. She is currently practicing in Chicago as the Chief of Ophthalmology of the Jesse Brown Veteran’s Administration while seeing pediatric patients at the University of Illinois at Chicago; she will join the faculty at the University of Pennsylvania/Children’s Hospital of Philadelphia this summer. Dr. Abbasian specializes in anterior segment disease in children with an emphasis on pediatric glaucoma and cataracts. She completed her ophthalmology residency at the University of Illinois at Chicago, her pediatric fellowship at the Children’s Hospital of Philadelphia, and her glaucoma fellowship at the University of Illinois at Chicago.
Download English Transcript PDF
MS. KACI BAEZ: Hello, and welcome to today’s BrightFocus Glaucoma Chat. My name is Kaci Baez, VP of Integrated Marketing and Communications at BrightFocus, and I’m excited to be here with you today as we talk about Childhood Glaucoma. Our Glaucoma Chats are a monthly program in partnership with the American Glaucoma Society designed to provide people living with glaucoma and their family and friends who support them with information straight from the experts. BrightFocus is committed to investing in bold research worldwide that generates novel approaches, diagnostic tools, and life-enhancing treatments that serve all populations in the fight against age-related brain and vision diseases. I would like to introduce today’s guest speaker, Javaneh Abbasian, MD. Dr. Abbasian is a board-certified ophthalmologist who is dual-fellowship trained in both pediatric ophthalmology and adult glaucoma. She is currently practicing in Chicago as the Chief of Ophthalmology of the Jesse Brown Veterans Administration Medical Center while seeing pediatric patients at the University of Illinois Chicago. She will join the faculty at University of Pennsylvania and Children’s Hospital of Philadelphia this summer. Dr. Abbasian specializes in anterior segment disease in children, with an emphasis on pediatric glaucoma and cataracts. Welcome, Dr. Abbasian. We’re so excited to have you here today.
DR. JAVANEH ABBASIAN: Thank you, Kaci, for the introduction and the invitation to be here. I’m really excited to share my experiences with all of you.
MS. KACI BAEZ: Okay, well, wonderful. So, our first question, let’s just dive right in by defining: What is childhood glaucoma, and what are the different types of childhood glaucoma?
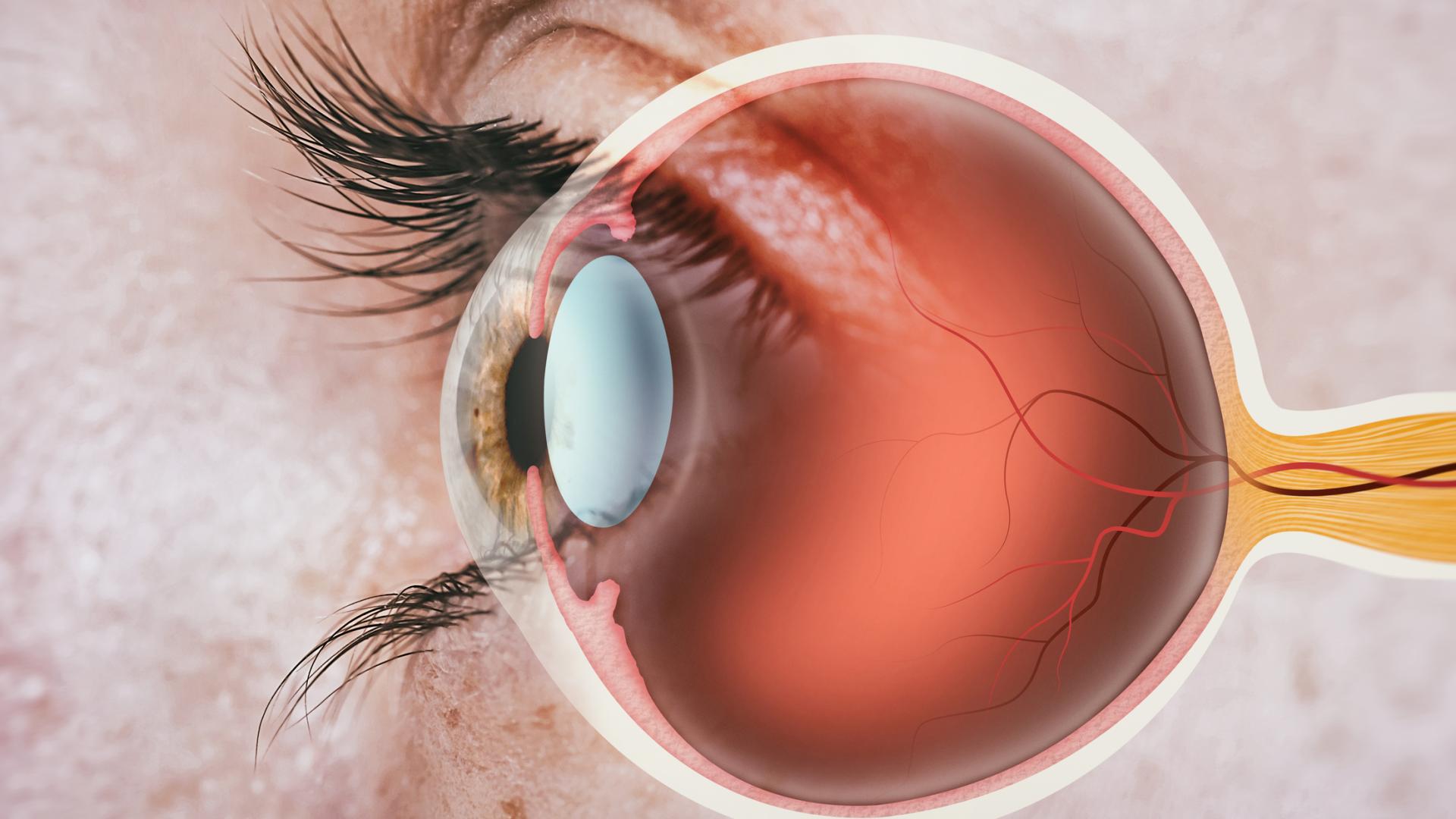
DR. JAVANEH ABBASIAN: Okay, great. Definitions are actually a really good place to start to make sure we’re all talking about the same thing. When most people think of pediatric glaucoma, they’re thinking of something called primary congenital glaucoma. And that is a group of diseases in early childhood that affect children that are 2 years or less in age. Ophthalmologists have further divided this into a neonatal onset—so, children that show signs of glaucoma at birth or within the first month of life—and then infantile glaucoma is children that are between 1 and 24 months. Beyond that, after the age of 2 years all the way up to 18 years of life—early adulthood—we call children that are affected with glaucoma as juvenile-onset glaucoma. So, those definitions tell us the category of the child we’re talking about and the type of disease we’re talking about, but just to give you a beginning framework of how to think about glaucoma, when I explain glaucoma to my pediatric patients and their parents, I describe it as an imbalance in the natural drain of the eye. If we think about the eye having its own fluid system, similar to water in a pipe that we’re all familiar with in our homes and so forth, in congenital glaucoma, there isn’t really a problem in producing the water. The problem, or the issue, is how the water exits the eye. And that system is very similar to a shower drain, and the pipes further beyond that take water out of the system. In primary congenital glaucoma and, to some extent, in juvenile-onset glaucoma, this group of diseases, the issue is either with the drain or with the pipes that go out or with both. And if we take the analogy even further, I would say that this buildup of water is like a buildup of pressure in the eye, which we’re all familiar with as we’re talking about glaucoma. And that pressure can cause damage to the eye if it’s not relieved and treated long term. So, that summarizes the definitions of the different types of glaucoma in the primary onset group and also how it behaves in the eye.
MS. KACI BAEZ: Okay. Great. Thanks for the explanation. And so, what are the signs and symptoms typically associated with these types of childhood glaucoma?
DR. JAVANEH ABBASIAN: The signs and symptoms of pediatric glaucoma, they’re interesting, and it’s actually a bit different in this way from adult glaucoma, because it’s happening to a young child in a growing eye. Oftentimes, there are symptoms that the parents see that they know something is wrong. One important one is light sensitivity. In some kids, the child will not open their eyes all day long; they’ll react very strongly when the lights are on and cry and scream. And other kids, they, kind of, forcefully open and close their eyes, which the term is called blepharospasm. And lastly, another symptom is profound tearing. That sometimes happens even when the child is not crying or they’re not upset. They’re just constantly tearing from their eyes—one or both. Those are symptoms. If those symptoms are not there, the caregiver may actually see physical signs that indicate that there is a change going on in the eye, and that is because of the high pressure. In those cases, the stress that the pressure causes in the eye makes the eye grow fast, and faster and in larger proportion than what we would expect from natural growth.
One typical thing that a parent will come in with is they will say that the cornea, which is the front part of the eye and is typically clear, has gotten very large very quickly—it’s very prominent. And in some cases, it happens so quickly, the pressure is so high, and the cornea is under quite a great amount of stress that it causes breaks in the cornea in some of the deeper layers. And then, an influx of water comes in and the cornea becomes cloudy, so the parents may say, “Now I can’t see the colored part or the iris in the eye anymore because all I see now is a white cornea in front of me,” and the child seems quite bothered by this. The last thing I’ll say that parents notice sometimes is that their kid is extremely irritable and, sometimes, inconsolable. So in those situations, parents may not know exactly what is going on, but they know something is wrong, and incidentally, when they get care and when the pressure is lowered, parents will remark that this is night and day, that their child is a completely different kid now that they’re comfortable and the pressure is relieved and, presumably, that the child is no longer in pain. So, these signs and symptoms are quite different from adult glaucoma in the sense that there may be something visible or something that the parents notice that is out of normal for what the child has typically been experiencing.
MS. KACI BAEZ: You answered my question. I was going to ask if there was ever an instance where there weren’t any vision symptoms at all, because that does happen with adults.
DR. JAVANEH ABBASIAN: Yeah, that is a great question. I mean, sometimes I think that the parents will recognize that something is not right. And like we talked about, if any of those tearing and light sensitivity, all those things are not there, it may also be the kid’s attitude that something is not appropriate, and they may see something that looks a little bit atypical in the largeness of their eye. At times, which we can talk about afterwards, when a when a doctor is making a diagnosis, sometimes, to be honest, it’s a borderline case and there’s enough suspicion that the doctor would recommend an exam under anesthesia where certain measurements and things can be made to understand if the diagnosis is, in fact, there, because it may not be as obvious. What I was talking about are the more obvious instances in which the parents are aware that something is wrong.
MS. KACI BAEZ: Thank you. I know it can be overwhelming to parents trying to understand, you know, if their child may have an eye disease. And so, how would glaucoma—juvenile or childhood glaucoma—get diagnosed? And what type of doctor should concerned parents take their child to?
DR. JAVANEH ABBASIAN: That’s a great question. If any of the features we just talked about are present, then a lot of times the provider can make the diagnosis clinically. And the type of doctor to see, I’ll start from there, and then we can further talk about how it all unravels. I would say pediatric glaucoma is typically considered a surgical disease, so enlisting a surgeon in the care of the child is incredibly important as part of the care team. Interestingly, in ophthalmology, both pediatric-trained ophthalmologists and glaucoma-trained ophthalmologists are often those possessing the skills to treat this group of kids. So, depending on who is in your area, those would be two great specialists to try. In our health care system, when a child comes in for a well visit, typically we are still checking things that typically parents may see, like pressure and vision, and we’re looking at the eye and inspecting the front part of the eye and so forth. A lot of the things that we talked about that are a few standard deviations out of line—the cornea is too large, the child has a cloudy front part of the eye, they’re tearing a lot—a lot of these things would be very visible when we first walk into the room.
If, for whatever reason, we’re not able to understand what is happening, we can take the pressure with a bunch of automated contact instruments, and that may give us a clue if the pressure reading is very high. And often if a normal pressure in an adult is 20, 21, children actually run a lot lower, typically, and a child with glaucoma may come in with pressure of 30, 40, or 50, something like this. So, the instruments would help us understand that, as well. Lastly, I would say that even if all of those things don’t work, the skilled physician would be able to press on the eye using their fingers and detect that there’s a firmness to it, and that is an indication that the pressure is high. So, there are a number of ways in which in the office, hopefully, we can get closer to an understanding of what it is we’re looking at. And as I was mentioning before, if all else fails beyond that, then most providers would suggest an exam under anesthesia. And that can be scary, but the truth is that it is the easiest way sometimes to make sure that what we’re looking at is either normal or is on the spectrum of pathology or something being wrong with the eye. And so, we do it in that kind of controlled environment to make sure that we can confirm the diagnosis if it’s there.
MS. KACI BAEZ: All right, thank you. What causes glaucoma to occur in people under the age of 18? Is it genetic? Do we do we fully know what causes it?
DR. JAVANEH ABBASIAN: Yes, that’s a good question, too. What we’ve talked about so far are the primary congenital glaucomas, which are the ones that many people experience early onset in their children, and as we talked about, something is clearly wrong. And oftentimes, those are inherited, genetic problems. We don’t always know the answer, despite sending most of these children for genetic testing. And I personally try to send every patient that I have for genetic testing if I am confirming a diagnosis of glaucoma. The majority of those kinds of genetic abnormalities are sporadic, meaning that there isn’t a family history of this, but there are some cases in which it is inherited by family tree, and it oftentimes is recessive in those cases. Interestingly, in some ethnic groups the incidence of glaucoma is much higher. So, in some places you might see glaucoma in 1 in 2,500 people, and in other populations, it may be reported as 1 in 10,000 or 1 in 30,000. So, it’s quite a rare disease when it’s the lane of primary congenital glaucoma, and the genetics may help us get a bit closer to why this happened. But as we talked about earlier, it’s really a developmental problem; something just did not naturally occur to allow the fluid to get out of the eye, and the cause of that then becomes a high pressure that can cause damage to the kid in the future.
MS. KACI BAEZ: Thank you. Are there any other possible causes of glaucoma developing under the age of 18?
DR. JAVANEH ABBASIAN: Yes, I’m actually very glad you brought that up. Yes, there are. So, the categories beyond the ones we discussed—the primary congenital glaucoma and the juvenile-onset glaucoma—in my mind, there are two. And how I group them is that glaucomas that are associated with ocular diseases of the eye or conditions in the body that are systemic that can also affect the eye and cause glaucoma—that’s one category. And the second category is that something external has happened—so, either the child is on a medication that causes glaucoma or they’ve had surgery in the eye, etc. I’ll share with you a couple of names of some diseases that if the primary care doctor—pediatrician, neurologist, any of these people—have seen the child and know and have diagnosed them—this is like these systemic diseases—have diagnosed them with a disease, the ophthalmologist should be involved to also look and co-manage, anticipating a risk for glaucoma. Those diseases that come to mind are Sturge-Weber syndrome, Lowe syndrome, Axenfeld-Rieger syndrome, and then neurofibromatosis. Those are the ones associated with things going on in the body, as well.
For the ones in which something is going on with the eye, I would say the three big ones are aniridia, Peters anomaly, and retinopathy of prematurity that affects our youngest preemie babies. Those are the ones in which the child has other things going on in the eye or the body. For the external factors category, the things to include in which a child can acquire glaucoma is either they have inflammation in the eye, which we call uveitis, or some sort of inflammatory disease. Sometimes it happens because of the medications, and the big one here is steroid use, which can cause pressures to rise. If the child is unfortunate to have a tumor in the eye, then that can cause a problem with the drain, as well. And then, the broad category would be if the child has had other surgeries. And in the pediatric population, the biggest one for this is if they’ve had cataract surgery, primarily the early-onset type, and we call this category glaucoma following pediatric cataract surgery. I guess the reason that I bring all of these examples up is that if anybody falls into any of these categories, an ophthalmologist should be monitoring them, because they may not have glaucoma right away, but in the long term, it would be helpful for them to be watched by someone, observed in the event that they unfortunately get glaucoma.
MS. KACI BAEZ: Thank you. That’s so helpful to understand when there’s so many different types of glaucoma and so many possible causes. Regarding the relationship between adult and childhood glaucoma, would you be able to explain that a bit more for our listeners? For example, if someone has primary open-angle glaucoma that they developed later in their adult life, are their children and grandchildren at increased risk of developing a childhood glaucoma or being born with it?
DR. JAVANEH ABBASIAN: That’s a great question. And I’m sure it also highlights just how concerning this group of diseases are when people are confronted with the reality of having someone have it or having a relative with it and so forth, so really an important question to ask. How I would think about it is that they are, in fact, quite different, childhood glaucoma and adult-onset glaucoma. The children in their developing eye, something has gone wrong. And as we’ve kind of talked about, it might be genetic. It may be related to some other disease that they have in the eye or in the body. It may be something sporadic that we could not have anticipated that it’s happening, but that has caused an issue very early on with the pipe and the drain, and therefore, the pressure has gone up. That is very different than the type of adult-onset glaucoma that, even as an adult glaucoma specialist, as well, I experience in patients that are significantly older and could carry a bunch of different diseases, as well, of the eye that predispose them to glaucoma, but the truth is that they had a very functioning system for a number of years—decades, in fact—prior to the onset of their glaucoma. So, it’s better to think of them as two completely different subtypes of disease.
The one area in which family history would be important is in the juvenile-onset glaucomas. This is very clearly genetically driven, and in those kids that have this, there are a lot of reported cases of relatives and family members who have disease or high pressures and so on. So, in this case of juvenile-onset glaucoma, it is important to take a careful family history. Also, what comes to mind beyond this is that for the pediatric glaucoma patient, if they’re thinking ahead and they’re thinking about their adult life and the possibility of also having adult-onset glaucoma, how I would look at it is that it’s a continuum of the child’s eye disease. So, even if the eye disease is under control as a child and they’ve had a number of treatments and therapies and their pressure is good, they can still be affected by the same changes that happen in adulthood for patients with primary open-angle glaucoma of adulthood, and, perhaps even more so because they have a partially compromised system. But, typically, when we discuss patients in their adulthood who have a history of childhood glaucoma, we tend to think of it as a continuum. Even though they’re much older now, how it all started was related to a childhood onset.
MS. KACI BAEZ: Thank you. That’s so helpful. And so, some listeners may want to know: Does childhood glaucoma result in blindness? I guess that’s one big question people may have. And then, what is the typical treatment like for something like this?
DR. JAVANEH ABBASIAN: So, your first question is a very tough question to answer because we as providers would love for the answer to be that nobody results in blindness under the care of a health care provider. But the truth is that while the majority of cases, which is great, do not result in blindness when they’re under control, that can happen, and that is often in the most severe cases, of course, or in cases in which there isn’t good care or compliance with care. And so, how I would look at it is more that there’s a partnership between the provider and the patient and the parent to try to beat this thing and try to make sure that the child is seeing and at their best capacity for as long as possible, if not forever. But to your point, if it’s left untreated in places in which there’s not access to good care and so forth, this does result in blindness, because the pressure on the nerve—the optic nerve—is so great at some point that the vision will be diminished.
For some of the listeners who may be familiar with adult glaucoma, the medical treatments and the surgical treatments, many of them are quite similar. Many of these children have had surgery. As I was mentioning earlier, it’s primarily a surgical disease and has eye drop maintenance or by-mouth pills to supplement, as well. The range of this, of course, it matters what type of disease the child has and also the severity of the disease. So, some children may have undergone multiple surgical procedures, yet they still take three or four or five drops a day. And others may have had just one surgery; it was caught early; it was a less advanced type, a more simplistic type; and they take only one eye drop. So, the spectrum is quite great, and how most of us approach this is that it’s a very individual disease. We are familiar with all the different kinds of ways that glaucoma can present to us, but every child has a different presentation and has a different anatomy and requires different individualized care. And the bag of tricks will always include medical and surgical treatments to keep things under control.
MS. KACI BAEZ: Thanks for that information. I’m not sure what the latest stat is. The latest stat that I could find, according to the AAO [American Academy of Ophthalmology], is that there’s at least 300,000 cases of glaucoma in people under the age of 18. And I can imagine that that has to be scary, probably both for the parents but also for the child under the age of 18. And so, what resources are available regarding childhood glaucoma for the parents? And I’m not sure if there are any resources available for the children, as well—the affected individuals.
DR. JAVANEH ABBASIAN: Your stat is exactly right. That’s what’s been reported to us epidemiologically, that around 300,000 people are living with this currently. Regarding resources, there are many, which is great because a lot of times, as many can imagine, this is a very overwhelming scenario for parents. And sometimes, just debunking some of the opaqueness of what’s about to happen is helpful. So, the resources, or where I would start, is, of course, with BrightFocus and the American Glaucoma Society websites, which provide quite a bit of background in just understanding what is glaucoma and the mechanism of how high pressure affects the eye. They also go into various treatment strategies and so forth, and a lot of this is very applicable to the pediatric group as well; it’s quite broad. For pediatric-centered information, there are several groups of pediatric ophthalmologists and glaucoma ophthalmologists that have probably—I mean, I’ve not directly asked them this—but have probably seen the difficulty that the parents experience in making decisions without enough information, and they have taken it upon themselves to provide educational hubs and websites and so forth for their patients and for the parents.
A few websites that I would recommend, one is from the American Association for Pediatric Ophthalmology and Strabismus. There’s a nice tab for patients and educational materials, and there’s a good subheading there for pediatric glaucoma. There’s another wonderful network that some ophthalmologists started a little over a decade ago called the Childhood Glaucoma Research Network, and they have quite a bit of information online, as well, that can be helpful and useful, not only in background knowledge but also making decisions with the provider. The last one I would say, there is a family association. The title of the group is called Pediatric Glaucoma and Cataract Family Association. They have a website. They also have quite a bit of material that pertains to the disease, and certainly, if the child is of age where they can read, this will help them too. All this information—this one, particularly—will help them to familiarize themselves with what is happening. It is I would say, I think, this is one of the hardest things for parents and families from my observer view to see them not know what’s going to happen next. And that’s really scary with a kid. So, some of these resources prepare you even for going into the eye exam to discuss with the doctor. At least you have a little bit of background information to have a meaningful conversation that you can feel good about and advocate for your kid, as well.
MS. KACI BAEZ: Thank you so much. And this is a scary topic, childhood vision disease, as a parent, and it’s just really scary to think about the unknown if you want to help your child. You don’t want them to have any problems, so it’s really wonderful that there are so many resources available. And regarding my next question—it’s sort of related: What are some exciting advancements that could potentially be utilized in childhood glaucoma treatment or prevention?
DR. JAVANEH ABBASIAN: Yeah, I’m so glad that you asked this, because this is actually like an optimistic and important part of this conversation. The great news about all the advancements in the world of adult glaucoma is that many of them are either being considered or being utilized in the pediatric population—safely, of course. But as the explosion of medications and minimally invasive surgeries and new forms of devices hits the market, we who treat pediatric glaucoma are furiously taking notes on what are the profile of these new things, because something as simple, for instance, as medications is really difficult in children. An adult taking a medication one to five times a day is already a big ask, but to have to instill those eye drops in a child is difficult, but then three to five times a day in some of these families can be quite taxing. So to that end, there’s a lot of research now on how we can give medications as what we call a depot, so a large amount of medication is administered, but it releases itself frequently and in a sustained way over time. So, instead of instilling all of these eye drops every day, the goal or the hope would be that some of these vehicles—whether it’s a contact lens or a ring in the eye or something that we inject in the eye in a minimally invasive procedure—that it takes the burden off of the daily application of the medication and, instead, prolongs the life of that medicine in the eye for months. And that can be a real gamechanger for parents if that comes to fruition for children. That’s the medical route.
And in the surgical route, as many who are familiar with glaucoma may see, there’s a lot of new devices, and there’s a lot of strategies that are what we call minimally invasive to be utilized in the eye to treat glaucoma. And in some cases, with children who have a developmental problem with their drain and their pipes, this is actually a great strategy to use some of these devices in order to try to open the drain or produce more flow in the pipes. And we’re looking at the research, of course, over time to see how these new technologies bear out. But it’s a great innovation to be able to offer more strategies to this population, especially after it’s time tested in adults and can be seen as safe and efficient and efficacious and so forth. So, I am very optimistic that in the future we’ll be able to offer kids much more than we have at our disposal now because of all of this growth in the field of glaucoma, so we’re very fortunate for that.
MS. KACI BAEZ: Thank you so much. This has been such helpful information, and I just wanted to ask: Is there anything else you would like to share with our listeners regarding this topic, childhood glaucoma? Any tips or other parting wisdom?
DR. JAVANEH ABBASIAN: Yeah, that’s a really great final sendoff here. I would say that pediatric glaucoma is a very unfortunate set of diseases that can still produce a very good outcome, and the child can still do great things and have a great future despite having this disease or setback. It’s more about the parent or the child feeling like this is not something that is going to define their entire life and their future, but something that we can work on and work through to get them to be a productive and happy person throughout their future. It’s not a hopeless disease by any means; it’s just one that requires a little more strength to get through it.
MS. KACI BAEZ: Thank you so much, Dr. Abbasian, for all the important information that you shared with us today. To our listeners, thank you for joining our Glaucoma Chat. We hope you found it helpful. Don’t forget to visit our website, www.BrightFocus.org/glaucoma for a wealth of information and resources. Our next Glaucoma Chat will discuss the latest on glaucoma eye drops and what you need to know. This will be on Wednesday, July 10. Thanks, again, for joining us, and this concludes today’s BrightFocus Glaucoma Chat episode.
DR. JAVANEH ABBASIAN: Thanks, Kaci.
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Since its inception more than 50 years ago, BrightFocus and its flagship research programs—Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research—has awarded more than $300 million in research grants to scientists around the world, catalyzing thousands of scientific breakthroughs, life-enhancing treatments, and diagnostic tools. We also share the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.

In this chat, Dr. Poonam Misra addresses some of the most common questions listeners have shared over the past year—from treatment options and lifestyle considerations to the latest educational resources.

Dr. Astrid Werner explains what causes dry eye, how to recognize the symptoms, and effective treatment options—including preservative-free drops, artificial tears, and eyelid care routines.
Join us for a fascinating conversation with Dr. Lucy Q. Shen as we explore cutting-edge research into restoring vision loss from glaucoma.

Preparing ahead of time can help you best manage your vision health. Here are some questions you can take along when you visit the eye doctor.
Support Groundbreaking Glaucoma Research
Your support helps fund critical research that could prevent vision loss, provide valuable information to the public, and cure this sight-stealing disease.
Donate Today