Breakthrough Study Creates Lab-Grown Eye Cells to Treat Macular Degeneration
Lab-grown cone photoreceptor cells respond to light, unlocking new potential for the treatment and study of macular degeneration.



Lab-grown cone photoreceptor cells respond to light, unlocking new potential for the treatment and study of macular degeneration.
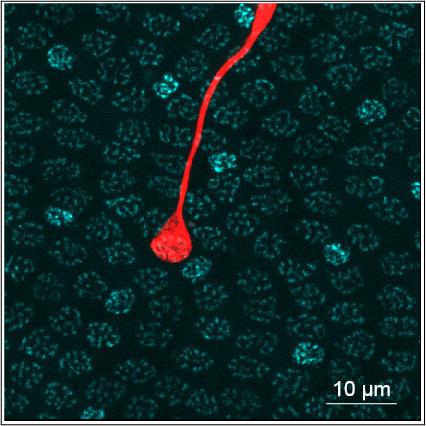
In a breakthrough that could mean potential new treatments for, a BrightFocus-funded research team has created first-of-its-kind laboratory-grown cone photoreceptor cells that respond to light. Cone photoreceptors are special cells that provide color vision and are responsible for converting light into signals that are sent to the brain.
They are located in an area of the retina called the fovea. Death of the foveal cone cells is the cause of blindness in many diseases, include age-related macular degeneration.
The research marks the first time that cone photoreceptors derived from adult stem cells showed the ability to respond to light, and the results could unlock new ways of studying and treating vision loss. The lab-created cells could eventually become replacements for human photoreceptor cells, restoring vision loss due to macular degeneration.
“Our everyday visual experience — including your ability to read this text — is dominated by signaling in a specialized region of the eye called the fovea, which constitutes an exquisite ‘high definition’ array of photosensors called cones that gives us humans a ‘high definition’ vision,” said the study’s senior author and BrightFocus Macular Degeneration Research grantee, Raunak Sinha PhD, professor of neuroscience at the University of Wisconsin School of Medicine and Public Health.
“Diseases that attack the fovea make it almost impossible to carry out everyday tasks such as reading, writing, driving, and recognizing faces. By providing the first detailed insight into how the sensors in the fovea work, we can devise treatments for eye diseases that affect the fovea and hence restore eyesight,” he added.
The study was published in the journal Cell Stem Cell.
Unlike many cells of the body, nerve tissue does not heal or grow back after it is damaged. This includes cells in the retina. A potential option that scientists are exploring is to replace dead cone photoreceptor cells with healthy cells created using stem cell technology.
A type of stem cell called pluripotent, which means it has the potential of taking on many forms in the body, can be sampled from adult skin and other tissues. Human pluripotent stem cells (hPSCs) can develop into any cell type, given the right growth conditions. This discovery has spurred numerous efforts to grow healthy tissues in a laboratory to replace diseased tissues in the body.
The research team refined a method for making retinal organoids, patches of tissue grown in a lab for eight or nine months until they produced mature rod and cone photoreceptor cells. A third of the mature cone cells responded to light of varying color and intensity, similar to cone cells in the human retina.
The created cone cells distinguished between green, blue, and red light — the way cells in the eye do. The response was proportional to light intensity and adapted to changes in background lighting, indicating that these cells contained the complex machinery needed for adjusting their activity.
BrightFocus-funded researchers including the University of Colorado’s Maria Valeria Canto-Soler, PhD, and others have pioneered the earliest “retina-in-a-dish” model to study age-related macular degeneration. However, the cells in retinal organoids demonstrated little or no ability to respond to light.
This newer study demonstrates for the first time that cone cells grown from human pluripotent stem cells can have a significant light response. In addition to unlocking new ways of treating vision loss from age-related macular degeneration, the cone cells also could serve as models for testing new drug treatments and for studying retinal degenerative diseases in the laboratory.
BrightFocus Foundation is a premier global nonprofit funder of research to defeat Alzheimer’s, macular degeneration, and glaucoma. Through its flagship research programs — Alzheimer’s Disease Research, Macular Degeneration Research, and National Glaucoma Research— the Foundation has awarded nearly $300 million in groundbreaking research funding over the past 51 years and shares the latest research findings, expert information, and resources to empower the millions impacted by these devastating diseases. Learn more at brightfocus.org.
Disclaimer: The information provided here is a public service of BrightFocus Foundation and is not intended to constitute medical advice. Please consult your physician for personalized medical, dietary, and/or exercise advice. Any medications or supplements should only be taken under medical supervision. BrightFocus Foundation does not endorse any medical products or therapies.
