Explore key milestones and see how our researchers are improving lives.
1979
National Glaucoma Research, a program of BrightFocus Foundation, begins.
2010
Grantees create the first noninvasive technique to measure eye pressure.
Grantee Joel Schuman, MD, and his team create the first noninvasive technique to measure eye pressure—the most important factor to consider in glaucoma. For the first time, scientists can visualize and measure how fast drainage in the front of the eye occurs without touching the eye and without any bright lights.
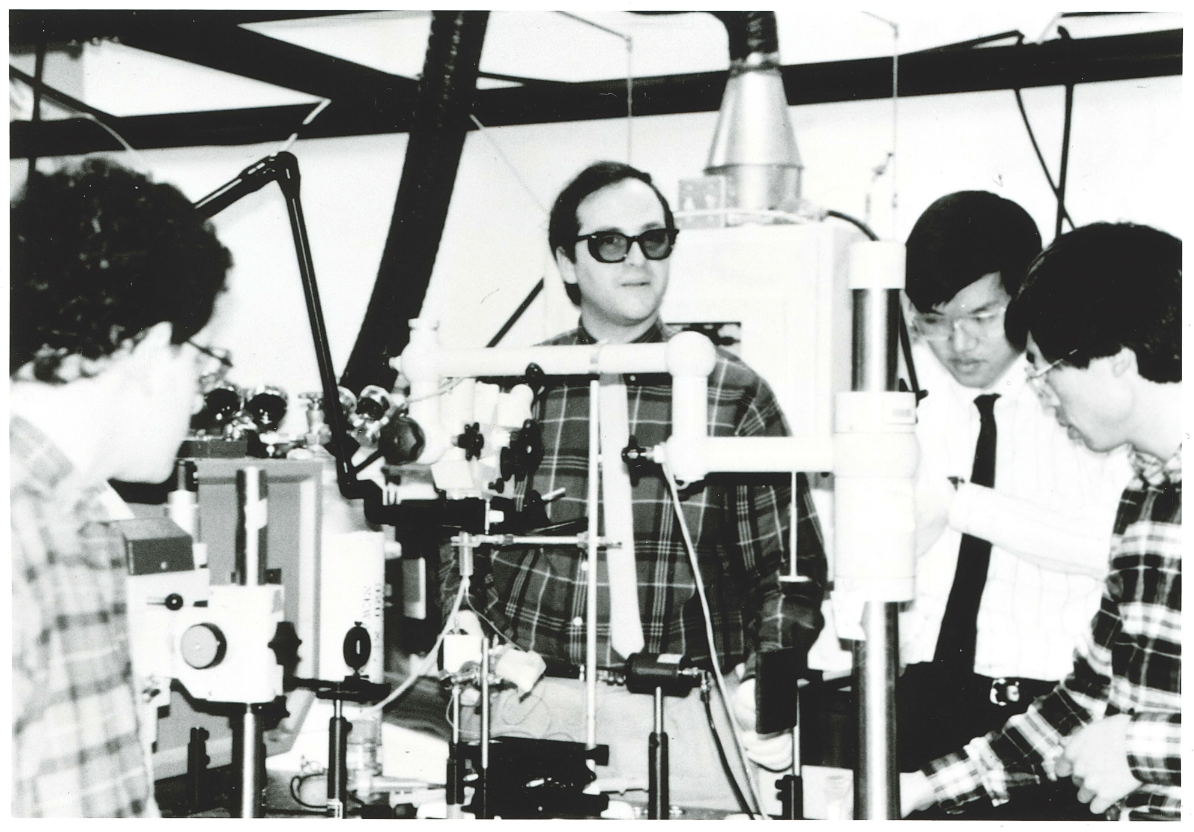
Dr. Joel Schuman (center) and his team circa 1995.
2010
Grantees create the first noninvasive technique to measure eye pressure.
Breaking Ground in Glaucoma: Spotlight on Dr. Joel Schuman
In 1995, with his ophthalmology residency a few years behind him, Joel S. Schuman, MD, received a BrightFocus grant to delve into the genetics of glaucoma. And before a decade passed, he and his colleagues were the first to identify a molecular marker for human glaucoma.
With several BrightFocus projects, Schuman has led research to develop advanced imaging for glaucoma and other vision diseases, which has led to advances in detection and early treatment.
Most notably, Schuman was a member of the team that developed a groundbreaking medical imaging procedure called optical coherence tomography (OCT) that creates a 3D map of the eye. This quick and noninvasive procedure allows ophthalmologists to measure the thickness of the optic nerve and to assess the nerve and surrounding tissue for signs of stress caused by pressure elevation. OCT is rapidly becoming the practice standard for diagnosing glaucoma and monitoring its progression. It makes it possible to intervene and reach treatment decisions earlier and is invaluable in helping to preserve precious sight.
“I cannot tell you how many times I’ve heard, ‘If it weren’t for BrightFocus, I could never do this research,” said Dr. Schuman. “What’s especially valuable about the BrightFocus mission is its focus on young investigators,” he continued. “They are our future, and BrightFocus has the foresight to invest in them, as the organization invested in me.”
“I have been privileged to be involved in research that has made a difference in people’s lives around the world. This would not have been possible without BrightFocus.”—Dr. Joel Schuman
2015
First clinical trial to test a new glaucoma treatment focused on neuroprotection and vision restoration.
Grantee Jeffrey Goldberg, MD, PhD, leads a BrightFocus-funded, first-of-its-kind Phase 2 clinical trial to test a new glaucoma treatment consisting of an experimental cell therapy to protect the optic nerve. In this innovative approach, a capsule is implanted in the eye that delivers a steady stream of growth factors to protect damage to the optic nerve, which could possibly improve vision in patients with glaucoma.

Dr. Jeffrey Goldberg
2016
First-ever creation and treatment of retinal ganglion cells using adult skin cells.
Grantee Jason Meyer, PhD, and colleagues reach a major milestone by creating and treating retinal ganglion cells (RGCs) derived from the skin cells of people with glaucoma. Healthy RGCs are crucial for vision, and this method could lead to treatments that prevent vision loss in glaucoma better than pressure-lowering treatments alone.
Watch a video featuring Dr. Meyer explaining his research.
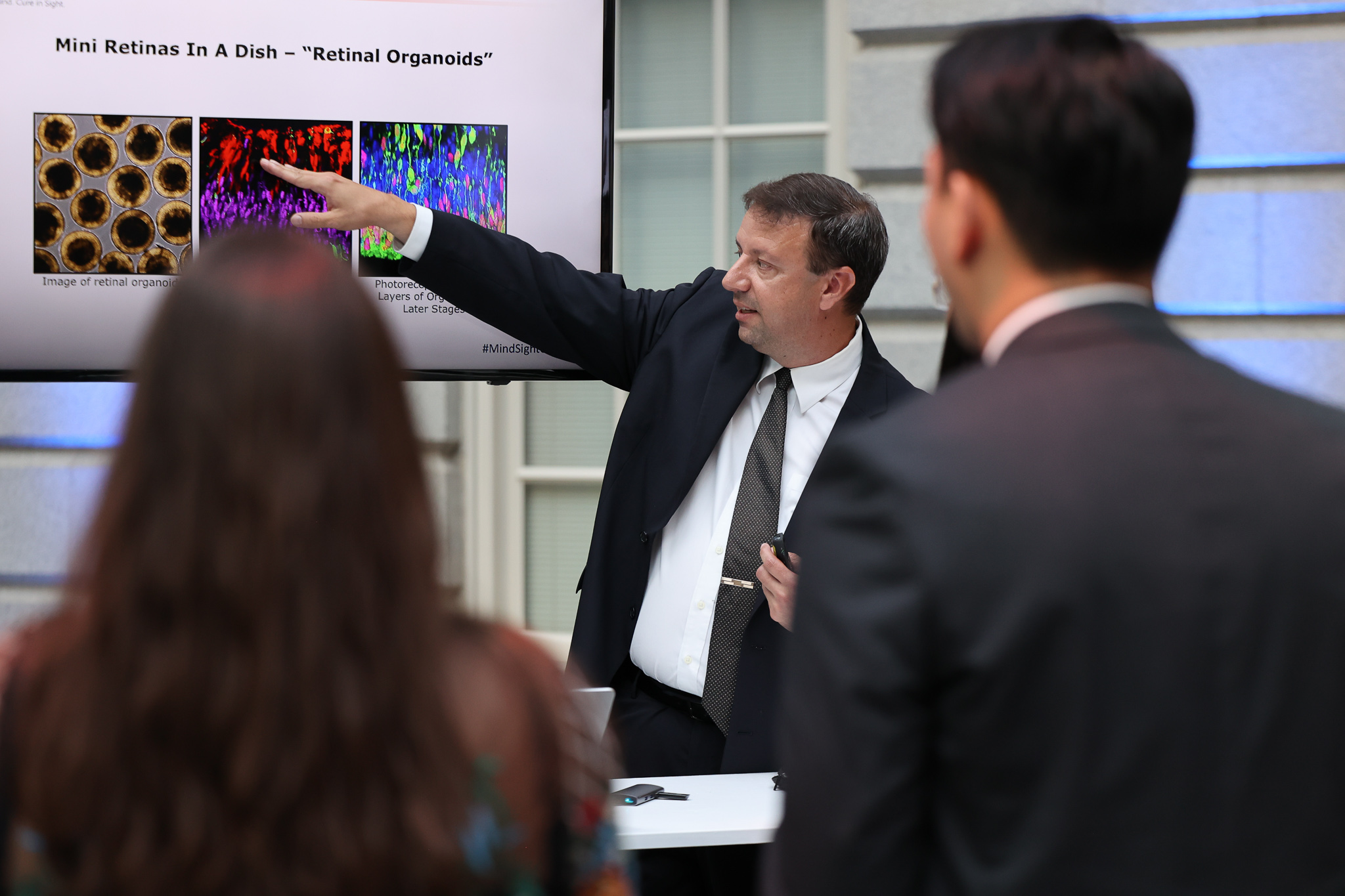
Dr. Jason Meyer presents his research at BrightFocus’ gala in June 2022.
2016
First-ever creation and treatment of retinal ganglion cells using adult skin cells.
2017
New class of glaucoma medication available.
The launch of Rhopressa, the first approved rho-associated protein kinase (ROCK) inhibitor—fueled by early BrightFocus-funded research—represents the first entirely new class of glaucoma medication to become available in more than two decades, since the first prostaglandin analog drug was approved in 1996. Early work by BrightFocus grantee Haiyan Gong, MD, PhD, proved this class of drugs could relieve eye pressure.
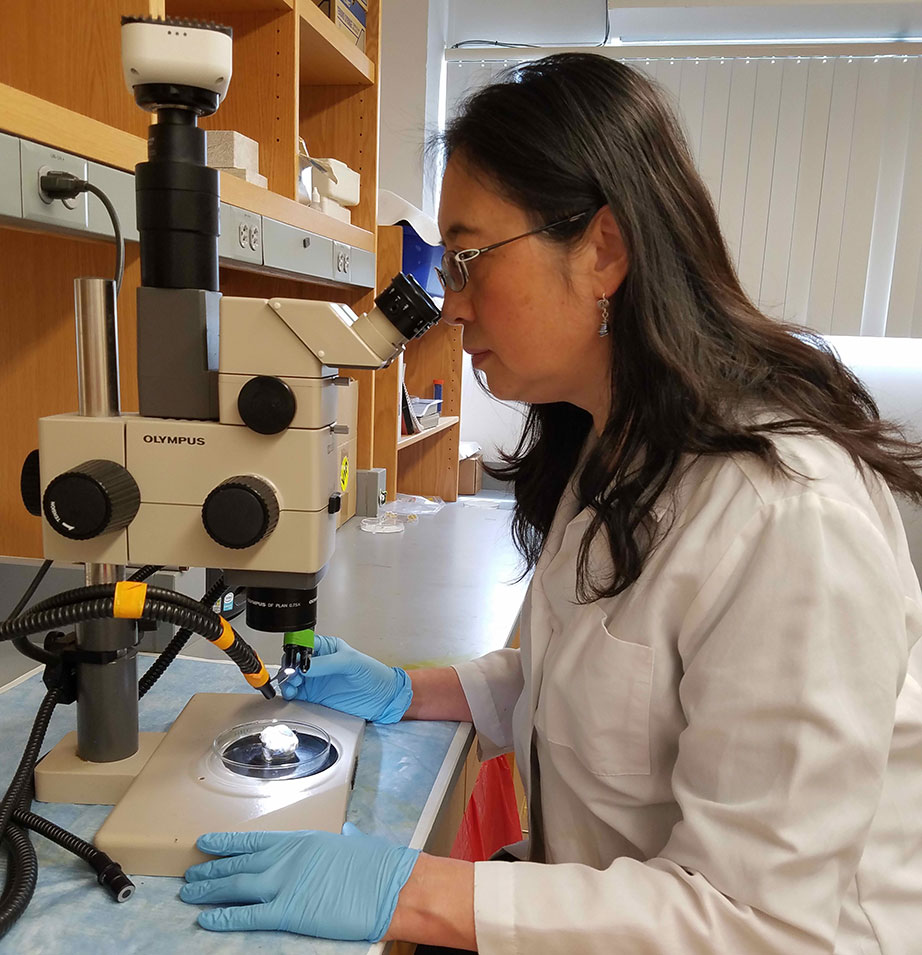
Dr. Haiyan Gong
2021
First successful cell transplantation gives hope for new glaucoma treatment.
Researchers, including grantee Petr Baranov, MD, PhD, and team at Harvard Medical School, successfully transplant—for the first time—lab-grown retinal ganglion cells derived from induced pluripotent stem cells into the eyes of mice. Based on this work, researchers estimate that people with late-stage glaucoma could begin receiving vision-restoring transplants in the next 10 years.
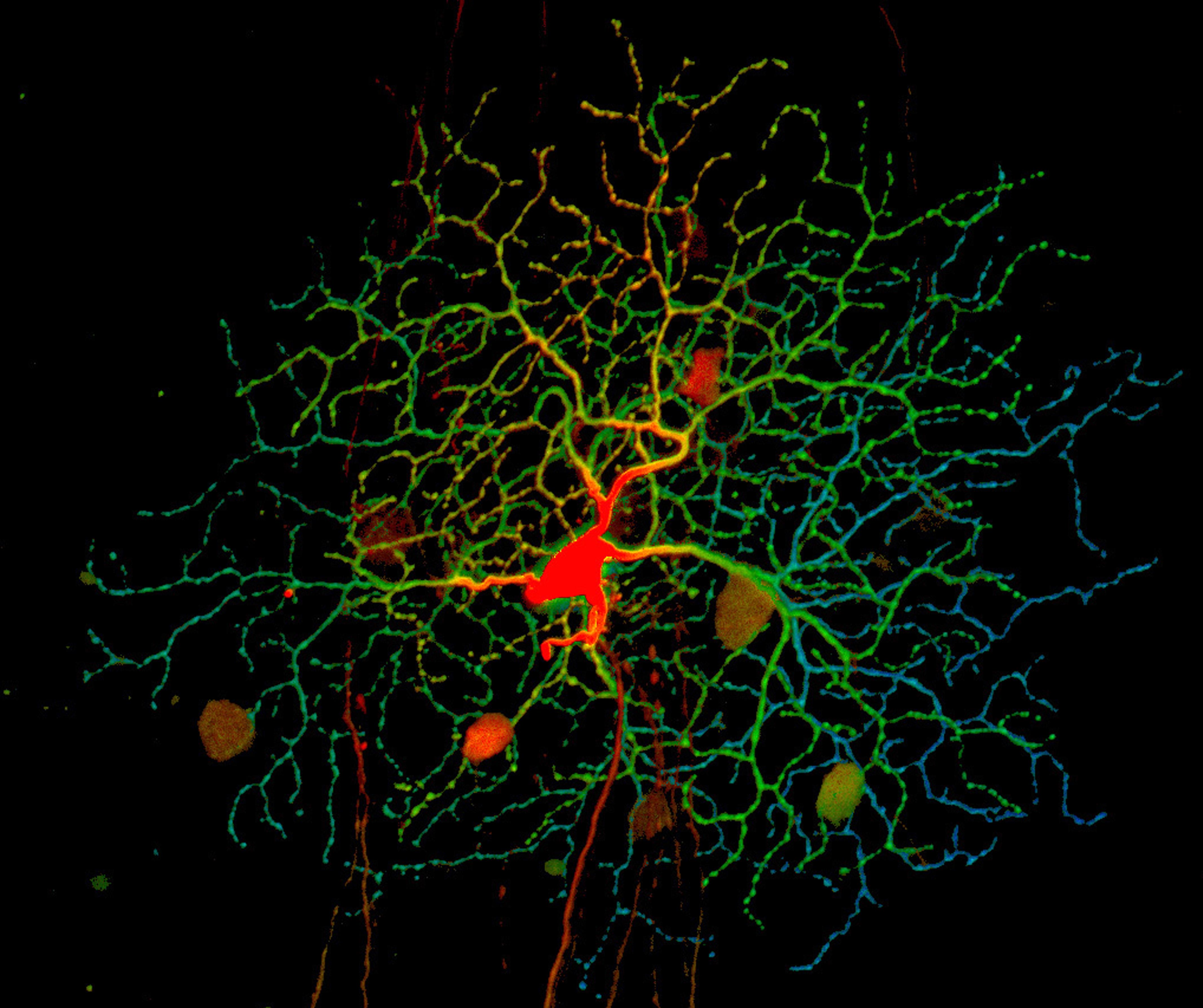
Retinal ganglion cells (blue, green, and red) receive information about the light our eyes detect from other cells in the retina at structures called dendrites (red) and then relay it to the brain via axons. Credit: National Eye Institute, National Institutes of Health (NEI/NIH)
2021
First-ever reversal of age-related vision loss and eye damage from glaucoma in mice.
For the first time, BrightFocus grantees and Harvard scientists Bruce Ksander, PhD, and Meredith Gregory-Ksander, PhD, successfully reprogram cells in mice to reverse vision loss from glaucoma, as well as normal vision loss associated with aging. The results show strong promise of gene therapy to reprogram eye tissue to restore vision lost to glaucoma and reverse aging and age-related diseases in humans.
“Meredith and I both got our start in glaucoma research from BrightFocus grants. We’ve received significant support over the years from your Foundation, and I am absolutely certain this project would not have been possible without this generous support.”—Dr. Bruce Ksander

Meredith Gregory-Ksander, PhD, and Bruce Ksander, PhD
2021
Researchers develop a new wireless device to diagnose and monitor glaucoma.
BrightFocus-funded scientists including J. Crawford Downs, PhD, develop a new implantable device that could change the way glaucoma is diagnosed. The wireless device measures intraocular eye pressure and a variety of pressure parameters in the eye.
Dr. J. Crawford Downs